Easy Treatment of Hypertension

Treatment of hypertension involves lifestyle changes and drug therapy. The ambition of antihypertensive therapy is to arrest morbidity and mortality affiliated with agilely raised BP by lowering it to the target level, with minimum inconvenience to the patient. Both systolic and diastolic BP predicts the likelihood of target organ damage (TOD) and complications such as:
- Cerebrovascular disease, transient ischaemic attacks, stroke, encephalopathy.
- Hypertensive heart disease-left ventricular hypertrophy, heart failure.
- Coronary artery disease (CAD), angina, myocardial infarction (MI), sudden cardiac death
- Arteriosclerotic peripheral vascular disease, retinopathy.
- Dissecting aneurysm of the aorta.
- Glomerulopathy, renal failure.
Patients who have already suffered some TOD have greater risk of further organ damage and death at any level of raised BP than those without TOD. The current NICE guidelines (2011) have graded hypertension as:
Blood pressure
| Hypertension | Systolic | Diastolic |
| Stage I | 140-159 | 90- 99 |
| Stage II | 160-179 | 100-109 |
| Severe | ≥ 180 | ≥ 110 |
Since the risk of complications depends not only on the level of BP but also on other risk factors (see box) and existing TOD, these have also to be considered in the selection of drugs and in devising therapeutic regimens.
Cardiovascular risk factors
- Age > 55 years (men), > 65 years (women)
- Family h/o premature CV disease
- Smoking
- Dyslipidemia (↑LDL, ↓HDL, ↑TG)
- Diabetes mellitus
- Hypertension
- Obesity (BMI ≥ 30)
- CKD (Microalbuminuria or g.f.r. < 60 ml/min)
- Sedentary lifestyle
CKD-Chronic kidney disease.
The JNC7 have also identified compelling indications (see box) which may mandate the use of specific antihypertensive drugs even in patients with BP values lower than 140/90 mm Hg. Moreover, the presence of compelling indications may suggest fixing a lower target BP value to be attained by drug therapy.
Compelling indications for specific antihypertensive drug classes
Diuretics
- Heart failure
- High coronary artery disease risk
- Recurrent stroke prevention
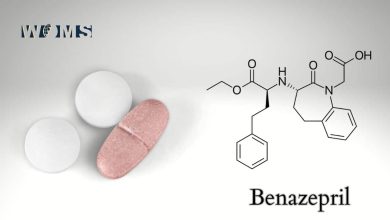
ACE inhibitors/ARBS
- Heart failure
- Post-myocardial infarction
- High coronary artery disease risk
- Diabetes
- Chronic kidney disease
- Recurrent stroke prevention
Calcium channel blockers
- Diabetes
- Stroke prevention
β – Adrenergic blockers
- Stable heart failure
- Post-myocardial infarction
- High coronary artery disease risk
Beneficial effects of lowering BP has been established in all patients having BP above 140/90 mm Hg, and even in the 120-139(systolic) or 80-89 mm Hg (diastolic) range in those with compelling indications or cardiovascular risk factors; e.g. in diabetics, lowering diastolic BP to 80 mm Hg was found to reduce cardiovascular events to a greater extent than on reducing it up to 90 mm Hg.
However, for patients aged ≥60 years the JNC 8 (2014) has suggested threshold systolic BP value of 150 mm Hg for initiating treatment, as well as to be the treatment goal (< 150 mm Hg). The threshold and goal diastolic BP value of 90 mm Hg is the same as for patients <60 years ago. Data from several large studies have shown that effective use of antihypertensive drugs reduces the occurrence of stroke by 30-50%, heart failure by 40-50% and coronary artery disease (CAD) by ̴15%. If the cause of hypertension can be identified (hormonal, vascular abnormality, tumour, renal disease, drugs) all efforts should be made to remove it.
Nonpharmacological measures (lifestyle modification-diet, Na restriction, aerobic activity or exercise, weight reduction, moderation in alcohol intake, mental relaxation, etc.) should be tried first and concurrently with drugs. When significant cardiovascular and/or renal damage has already occurred, lowering BP to normotensive level may not be tolerated: oedema, CHF, angina, rise in blood urea and syncope may be precipitated. Therefore, BP reduction should be gradual and only to the level tolerated.
Selection of antihypertensive drug/ combination
In the past, evaluation of thiazide diuretics, β blockers, ACE inhibitors/ARBs and CCB5 in large randomized trials with morbidity and mortality endpoints, established these drugs first-line antihypertensive drugs.
However, the latest hypertension treatment guidelines (JNC 8, NICE 2011) have excluded β blockers from the list of first-line drugs due to their lower efficacy in primary prevention of MI and stroke as well as other drawbacks.
A stepped care approach, initially using a single drug and progressively adding one or more drugs from different groups according to need, is recommended by most experts and therapeutic guidelines.
Step 1 The drug to initiate therapy is selected on the basis of compelling indications (if present); but for the majority of hypertensive patients who have no compelling indication, age and race have been recognized as a valid basis for selecting the initial medication. Because young (< 55 years) non-black subjects generally have higher plasma renin activity, they respond better to ACE inhibitors/ ARBS, while older patients and blacks of any age have lower renin status and show a weaker response to ACE inhibitors/ARBs.
Accordingly, JNC8 recommend initiating antihypertensive therapy with any one of a thiazide diuretic, or ACE inhibitor/ARBS or CCB for young (< 55 years) non-blacks, but the options for blacks of any age and older non-blacks are either thiazide or CCB. Since thiazide diuretics, even in low doses (12.5-25 mg/day), have an adverse (though minimal) metabolic profile, the NICE guidelines recommend only ACE inhibitor/ARB for young patients and CCB for older patients as well as for all blacks.
Diuretics may be used as alternatives to CCBS in patients not tolerating CCBS and in those with oedema or heart failure In women with childbearing potential and in those young hypertensives who have another contraindication to ACE inhibitor/ARB or are intolerant to these drugs, a β blocker may be used as the initial drug.
Step 2 When the target BP is not attained by a single drug a combination of two drugs, i.e. ACE inhibitor/ARB + CCB or diuretic if CCB not suitable, is recommended irrespective of the age or race of the patient. In selected cases where therapy has been initiated with a β blocker, the second drug should be a CCB.
Combination of β blocker with a diuretic is to be avoided because this increases the risk of developing diabetes. Initiating antihypertensive therapy with two drugs is advised by JNC8 in case the BP at diagnosis is >20 mm Hg systolic and/or >10 mm Hg diastolic higher than the goal BP.
Step 3 Treatment includes all 3 first-line drug classes, viz. ACE inhibitor/ARB + CCB + diuretic. However, before adding the third drug, the dose of existing medication should be titrated to the optimal or the best tolerated.
Step 4 Patients who do not achieve target BP even when taking optimal doses of 3 drugs are regarded as having resistant hypertension. Many patients having diabetes and/or CKD fall in this category. In such cases the NICE recommend adding a fourth drug, which can either be an aldosterone antagonist (if serum K+ is <4.5 mmol/L) or higher dose of the thiazide (if serum K+ is >4.5 mmol/L) or a β blocker (especially β blocker with vasodilating property, viz. carvedilol, nebivolol) or a selective α1 blocker. Only a few patients are likely to still remain uncontrolled. They require further evaluation and possible use of reserve drugs.
Antihypertensive combinations to be avoided
- An α or β adrenergic blocker with clonidine: apparent antagonism of clonidine action has been observed.
- Hydralazine with a DHP or prazosin; because of a similar pattern of haemodynamic action.
- ACE inhibitor with an ARB.
- Verapamil or diltiazem with β blocker, because marked bradycardia, A-V block can occur.
- Methyldopa with clonidine or any two drugs of the same class
- β blocker with a diuretic, because of increased risk of developing diabetes.
Some antihypertensive combinations
- Amlodipine 5 mg + Lisinopril 5 mg-AMLOPRES-L, LISTRIL-AM
- Amlodipine 5 mg + Atenolol 50 mg-AMCARD-AT, AMLOPIN-AT, AMLOPRES-AT
- Amlodipine 5 mg + Enalapril 5 mg-AMACE, AMTAS-E
- Atenolol 25 mg or 50 mg + chlorthalidone 12.5 mg-TENOCLOR, TENORIC
- Enalapril 10 mg + Hydrochlorothiazide 25 mg-ENACE-D, VASONORM-H
- Ramipril 2.5 mg + Hydrochlorothiazide 12.5 mg-CARDACE-H
- Losartan 50 mg + Hydrochlorothiazide 12.5 mg-LOSAR-H, TOZAAR-H, LOSACAR-H
- Lisinopril 5 mg + Hydrochlorothiazide 12.5 mg-LISTRIL PULS, LISORIL-HT
- Losartan 50 mg + Ramipril 2.5 mg or 5 mg-TOZAAR-R, LAPIDO-R
- Losartan 50 mg + Amlodipine 5 mg-AMCARD-LP, AMLOPRESS-Z, LOSACAR-A
- Losartan 50 mg + Ramipril 2.5 mg + Hydrochlorothiazide 12.5 mg-LOSANORM-HR
- Irbesartan 150 mg + Hydrochlorothiazide 12.5 mg-IROVEL-H, XARB-H.
When the BP has been well controlled for >1 year, stepwise reduction in dose and/or withdrawal of one or more components of a combination may be attempted to work out a minimal regimen that will maintain the target BP. However, in most patients of essential hypertension, drug therapy is usually life-long.
Hypertension in pregnancy A sustained BP reading above 140/90 mm Hg during pregnancy has implications both for the mother and the foetus. Reduction of BP clearly reduces risks. Two types of situations are possible.
- A woman with preexisting chronic hypertension becomes pregnant.
- Pregnancy-related hypertension: as in toxaemia of pregnancy-preeclampsia: BP rises after 20 weeks of gestation.
Toxaemic hypertension is associated with a hyperadrenergic state, a decrease in plasma volume
(despite oedema) and an increase in vascular resistance. In the first category, the same therapy instituted before pregnancy may be continued. However, one of the ‘safer’ drugs listed below may be substituted if one of the ‘drugs to be avoided’ was being used.
The BP should be gradually reduced to a target level of <150 mm Hg systolic and 80-100 mm Hg diastolic, but drastic reduction should be avoided, because this may impair uteroplacental blood flow. Women with diabetes, CKD, chronic hypertension and history of a rise in BP during earlier pregnancy are at higher risk of developing preeclampsia.
To reduce the risk aspirin (80-100 mg/day) should be given from the 12th week of gestation until the baby is born. Aspirin is believed to prevent toxaemia by inhibiting TXA2 synthesis, which presumably plays a causative role.
Antihypertensives to be avoided during pregnancy.
ACE inhibitors, ARBS: Risk of foetal damage, growth retardation.
Diuretics: There is some evidence that by reducing blood volume, diuretics tend to accentuate uteroplacental perfusion deficit (of toxaemia)-increase risk of foetal wastage placental infarcts, miscarriage, stillbirth.
Nonselective β blockers: Propranolol has been implicated to cause low birth weight, decreased the placental size, neonatal bradycardia and hypoglycaemia.
Sod. nitroprusside: Contraindicated in eclampsia.
Antihypertensives for use during pregnancy
Labetalol This combined α + β adrenergic blocker (see p. 165) given orally is effective in the majority of cases and is most widely used now.
Nifedipine (sustained-release) This dihydro-pyridine CCB is a vasodilator that has been used in preeclampsia with good results. However, it should be stopped before labour begins, because it may weaken uterine contractions.
Methyldopa It has the longest record of use during pregnancy with safety and is still used. A positive Coomb’s test may occur but has no adverse implication.
Hydralazine This old vasodilator has been safely used during pregnancy but is not favoured now.
Hypertensive emergencies and urgencies
Systolic BP > 220 or diastolic BP> 120 mm Hg with evidence of active target organ damage (TOD) is labelled ‘hypertensive emergency’, while the same elevation of BP with symptoms, but no signs of acute TOD is termed hypertensive urgency’. Severity and rate of progress of TOD determine the seriousness of the condition.
Controlled reduction of BP over minutes (in emergencies) or hours (in urgencies) is required to counter the threat to organ function and life in the following situations:
- Cerebrovascular accident (haemorrhagic or ischaemic stroke) or head injury with high BP.
- Hypertensive encephalopathy (headache, confusion, irritability, disorientation, mental deterioration).
- Hypertensive acute LVF and pulmonary oedema.
- Acute coronary syndrome (ACS) or MI with raised BP.
- Dissecting aortic aneurysm.
- Acute renal failure with raised BP
- Eclampsia
- Hypertensive episodes in pheochromocytoma. cheese reaction or clonidine withdrawal
Parenteral drugs
Hypertensive emergencies require aggressive parenteral (preferably i.v.) therapy. Mean BP should be lowered by up to 25% over a period of minutes or maybe 1-2 hours, and then more gradually to not lower than 160/100 mm Hg. If the BP is reduced too quickly or too drastically perfusion of vital organs may suffer leading to impairment of kidney function, myocardial ischaemia, cerebral infarction, blindness, etc. Intravenous drugs with fast, predictable, titratable and short-lasting action are therefore required. Vasodilators acting directly on vascular smooth muscle (dihydropyridine CCBS, nitrodilators) and adrenergic blockers meet these requirements best.
1.Nicardipine This is one of the few DHPS available for parenteral (i.v.) use and has lately become the most popular drug for a variety of hypertensive emergencies, replacing nitroprusside. Nicardipine is highly vasoselective; primarily dilates arterioles.
As such reflex tachycardia may attend the fall in BP, to offset which a ß blocker like esmolol or labetalol should be coadministered when it is used in hypertensive emergencies attending MI or ACS Nicardipine is a short-acting DHP with rapid onset and offset of hypotensive effect after i.v. infusion. The fall in BP is predictable and dose-related. The elimination t½ on i.v. infusion is 45 mind action lasts for 3-4 hours. In clinical trials, i.v. nicardipine was as effective as nitroprusside in lowering BP in severe hypertension.
The target BP level was reached within 1 hour in >90% cases with both the drugs. Nicardipine has been found beneficial in both ischaemic as well as haemorrhagic stroke with raised BP. Its usefulness has been demonstrated in aortic dissection, acute heart failure and acute renal failure due to markedly raised BP, as well as
preeclampsia. Nicardipine infused I.V. is better tolerated and less toxic than nitroprusside. Adverse effects of nicardipine are mostly due to vasodilatation and are nonserious.
Dose: Initially 5 mg/hour i.v. infusion, increase the rate of infusion as needed up to 15 mg/hour.
NICARDIPINE HCI 25 mg/10 ml Inj.
Nicardipine has also been used in hypertension attending cardiac surgery and neurosurgery as well as to facilitate percutaneous coronary intervention.
- Sodium nitroprusside (see p. 613) Because of instantaneous, potent and combined arterio-venous vasodilatory action, nitroprusside has been a commonly used drug for hypertensive emergencies. However, the availability of less toxic and more manageable drugs has restricted its use. The major indication now is in cases of aortic dissection, where it is combined with the short-acting β1 blocker esmolol. It may also be used along with a loop diuretic in selected cases of acute hypertensive heart failure. Due to its potency and rapidity of action, nitroprusside needs a precise infusion pump and intra-arterial BP monitoring. Nitroprus side generates cyanide and thiocyanate which can produce CNS and other toxicities. In an ischaemic stroke, it may further compromise cerebral blood flow, while intracranial pressure may be further raised in haemorrhagic stroke. Nitroprusside is better avoided in these conditions.
- Glyceryl trinitrate (GTN) Infused i.v. (5-20 μg/min) GTN acts within 2-5 min but is not a potent hypotensive. Due to its pre-dominant vasodilator action, it is particularly suitable for use in MI or other ACS and in acute heart failure accompanied by a rise in BP. However, for any substantial lowering of BP, it needs to be combined with i.v. labetalol or i.v. nicardipine. Tolerance tends to develop to GTN action if it is continuously infused for >12 hours. GTN needs to be avoided in severe hypertension with ischaemic or haemorrhagic stroke.
4. Labetalol Unlike pure β blockers, this combined B and a-adrenergic blocker is an efficacious hypotensive when injected i.v. (see P. 165), and carries a low risk of causing excessive hypotension. It is particularly useful in lowering BP during episodes of the rise in BP in pheochromocytoma and other hyperadrenergic cheese reaction, cocaine abuse etc. Labetalol has been safely used in severe hypertension complicating aortic dissection, MI and other ACS, ischaemic stroke, intracranial haemorrhage and preeclampsia. It is good for patients with altered mental function because it does not cause sedation or increase intracranial pressure. However, heart failure and asthma preclude their use
Dose: 20-40 mg i.v. every 10 min till response or 20 mg/hour i.v. infusion, increased up to 120 mg/hour
LABESOL, LABETA 20 mg/amp. and 100 mg/amp. inj
- Esmolol This short-acting selective β blocker (see p.163) given as 0.5 mg/kg bolus i.V. injection followed by 50-200 Hg/kg/min i.V. infusion acts in 1-2 min, and the action lasts till 10-20 min after the infusion is terminated Esmolol is particularly useful when cardiac contractility and work is to be reduced, such as in aortic dissection. Nicardipine or nitroprusside is given concurrently because its BP-lowering action is weak. In MI/ACS complicated by raised BP and tachycardia, esmolol can be usefully combined with nicardipine or GTN. It needs to be avoided in the presence of systolic heart failure or asthma.
MINIBLOCK 100 mg/10 and 250 mg/10 ml inj. - Phentolamine This non-selective a, + a, adrenergic blocker (see p. 155) is an alternative drug to labetalol for hyperadrenergic states, e.g. hypertensive episodes in the- chromocytoma. Injected i.v. (5-10 mg) it accomplishment in 2 min and action lasts 5-15 min. Tachycardia and myocardial ischaemia may complicate its use, for which a B blocker may be added.
- Hydralazine Injected i.m. or i.v. slowly, hydralazine (see p. 612-13) acts in 20-30 min, and keeps BP low for 4-6 hours, but is less predictable. It is an alternative drug that has been particularly used for preeclampsia/eclampsia. It causes in patients with myocardial ischaemia or aortic dissection. A β blocker may be combined
- Furosemide (20-80 mg slow i.v.) This high ceiling diuretic (see Ch. 42) is not hypotensive, but may be given as a useful adjunct with any of the above drugs particularly vasodilators, if there is volume overload (in acute LVF, pulmonary oedema) or cerebral oedema (in encephalopathy). It needs to be avoided when the patient may be hypovolemic due to pressure-induced natriuresis (especially in eclampsia, pheochromocytoma). Fenoldopam (dopamine agonist), Clevidipine (ultrashort acting DHP) and enalaprilat (a parenteral ACE inhibitor) are the other drugs that are used in hypertensive emergencies but are not available in India.
Oral drugs
Oral hypotensive drugs that lower BP over a period of 2-48 hours may be more appropriate and safer in hypertensive urgencies when there is no immediate threat to life or of organ damage. The following oral drugs ave has been used:
1. Labetalol In a dose of 100-200 mg BD, it is a moderately potent hypotensive, that starts acting after 2- 4 hours and is satisfactory in many cases of severe hypertension without TOD. Labetalol is particularly suitable in preeclampsia, pheochromocytoma, stroke and ischaemic heart disease, but is contraindicated in the presence of heart failure.
2. Amlodipine This slow and long-acting DHP (see p.595) has been effectively and safely employed in many cases of severe hypertension, when raised BP is the only finding and there is no impending TOD or threat to life In a dose of 10 mg oral repeated after 12 hours and then once daily, it starts acting in 6-8 hours and may take 2-4 days to lower BP to target level. It is particularly suitable for elderly patients and those prone to postural
hypotension.
3. Captopril This non-prodrug, rapidly acting ACE inhibitor (see p. 530-31), has also been used orally (25 mg repeated as required) in hypertensive urgencies. Though it may lower BP in 30 min, the response is unpredictable both in intensity as well as in latency. It is not favoured now.
4. Clonidine Oral clonidine (100 ug every 1-2 hours) lowers BP within a few hours but produces sedation, dry mouth and rebound rise in BP on stopping. It is not suitable for the elderly and seldom used. Oral or sublingual use of immediate-release nifedipine capsules in hypertensive urgencies has been abandoned.