Pseudocyst of pancreas
Types I clinical features I investigations I treatment I complications
Pancreas: Pseudocyst and its types
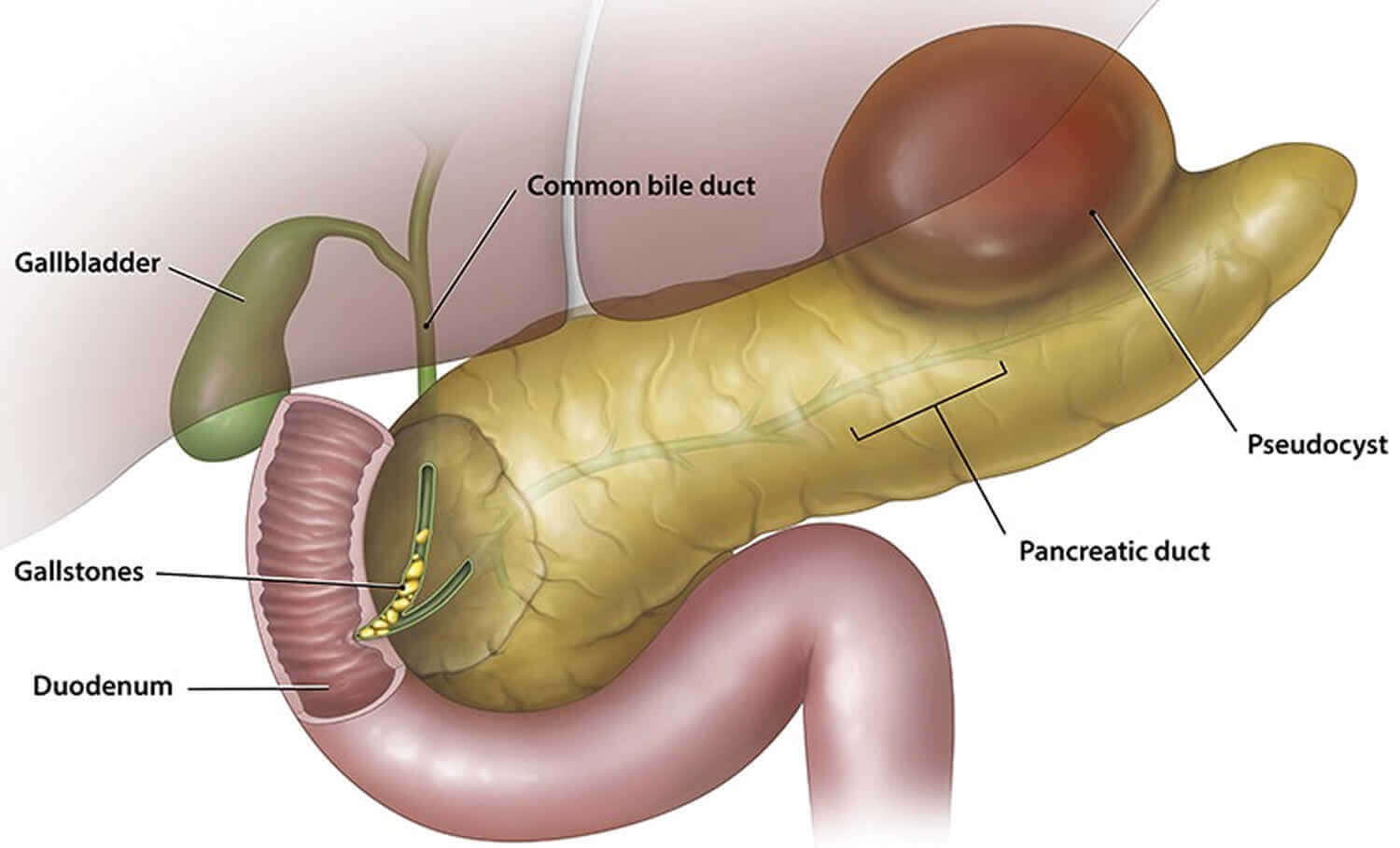
Pseudocyst of the pancreas or pancreatic pseudocyst is a localized collection of cloister pancreatic fluid, usually 3 weeks after the aggression of acute pancreatitis. It can develop after trauma and recurrent chronic pancreatitis.
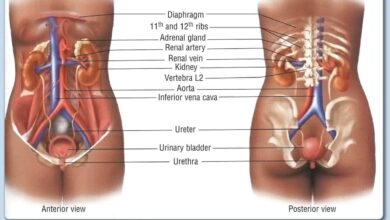
Accumulation usually occurs in the lesser sac in relation to the stomach but can occur in affiliation with duodenum, jejunum, colon, splenic hilum. About 50% of acute pancreatitis leads to pseudocyst formation, but among that 20-40% will resolve spontaneously.
Sites of pancreatic pseudocyst
The sites of pancreatic pseudocyst are given below:
- Lesser sac-accepted, i.e. between colon and stomach In relation to:
- Duodenum
- Jejunum
- Colon
- Splenic hilum
- Initially, the pancreatic cyst wall is thin (unformed), but later it gets fibrosed and thickened (formed) (matured).
- It is lined by fibrin layer but no endothelium hence called as pseudocyst
- It contains typically brownish fluid with sludge-like necrotic material. It can get infected to form infected pseudocyst or pancreatic abscess.
- Amylase level in the pancreatic cyst fluid is very high (>5000 units/ml)
Types of pancreatic pseudocyst
There are different types of pancreatic pseudocyst. Depending on whether it communicates with pancreatic duct or not it is classified as:
- Communicating pancreatic pseudocyst.
- Noncommunicating pancreatic pseudocyst
It can be
- Acute pancreatic pseudocyst.
- Chronic pancreatic pseudocyst.
D’Egidio classification of pseudocyst
A pseudocyst if, is classified on the basis of the etiology of pancreatitis i.e either it is acute or chronic pancreatic ductal anatomy if there is communication between the cyst and pancreatic duct then it is called D’egidio classification. The D’egidio classification of pseudocyst is given below:
- Type l: After an attack of acute pancreatitis. Normal duct anatomy; no fistula/communication.
- Type II: After an attack of acute on chronic pancreatitis. Abnormal duct anatomy without stricture; 50% chances of fistula.
- Type Ill: After an attack of chronic pancreatitis, abnormal anatomy with stricture; always communicating. It appears like a retention cyst.
Sarle’s classification
The Sarle’s classification is given below:
- Necrotic pseudocyst in acute pancreatitis.
- Retention cyst in chronic pancreatitis.
- Intrapancreatic retention due to pancreatic duct dilatation.
- Extrapancreatic retention cyst due to rupture into peripancreatic tissues.
Nealon and Walser classification
Based on the management of pseudocyst there is the importance of ductal anatomy. So, on the basis of this Nealon and Walser’s classification was developed. The Nealon and Walser classification is given below:
- Normal duct; no duct communication into pseudocyst.
- Normal duct with communication.
- Normal duct with stricture without communication.
- Normal duct with stricture with communication.
- Normal duct with abrupt duct termination.
- Chronic pancreatitis without duct cyst communication.
- Chronic pancreatitis with duct cyst communion.
Note:
- It is not a true cyst as there is no epithelial lining.
- 75% of cystic lesions of the pancreas are pseudocysts; Others are-cystadenomas, IPMNs, cystic necrosis of adenocarcinoma, congenital polycystic disease.
Clinical Features
Some of the clinical features are given below:
- Swelling in the epigastric region which is hemispherical, smooth, soft, not moving with respiration, not ambulatory, the upper margin is diffuse but lower margin well defined, resonant or impaired resonant on percussion, with transmitted pulsation confirmed by knee-elbow position.
- If it is infected, it will be tender mass and the patient will be toxic with fever and chills.
- Because the stomach is stretched towards the abdominal wall, Ryle’s tube passed will be felt per abdominally (Baid test).
Differential Diagnosis
Here are the differential diagnosis given below:
- Aortic aneurysm.
- Retroperitoneal cyst or tumor.
- adenocarcinoma of the pancreas.
- Cyst of the liven
- Mesenteric cyst.
- Hydatid cyst.
Investigations
We must have a clear idea of the pancreatic pseudocyst to know how to deal with it. We can investigate it by given following ways:
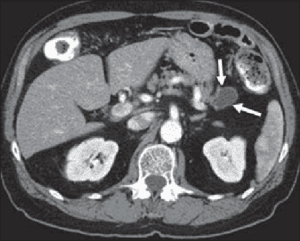
- US abdomen (commonly done the procedure), the US reveals the size and thickness of the pseudocyst. Size less than 6 cm indicates that one can wait for spontaneous resolution. Endosonography (EUS) is very useful.
- CT scan is ideal and study of choice. It is two times more sensitive than the US. It manifests size, shape, number, wall thickness, contents, pancreatic duct size, and ambit of necrosis in pancreas, calcification, and atrophy in chronic pancreatitis, regional vessels, pseudoaneurysm, splenic/portal vein thrombosis.
- MRCP delineates the ductal anatomy and its abnormality.
- ERCP is done to find out the communication.
- Barium meal (lateral view) shows a widened vertebrogastric angle with a displaced stomach (Not usually done now).
- LFT, serum amylase platelet count, PT INR.
- EUS-guided aspiration and analysis of fluid for amylase and CEA. Amylase will be high with normal CEA in pseudocyst; amylase will be normal/low with high CEA >400 ng/ml in mucinous neoplasm.
Treatment of pancreatic pseudocyst
Pancreatic pseudocyst can be treated. The treatment of pancreatic pseudocyst is given below:
- Conservative-Observation, follow-up using repeat USG at regular intervals. 50% of pseudocysts show spontaneous resolution.
- Interventional-Needs ERCP to delineate ductal anatomy, pancreatic duct stones, mainly communication into the pseudocyst, It is Guided—Endoscopic/EUS/US-guided drainage
- Transpapillary-Through side-viewing endoscopy, pancreatic sphincterotomy is done; guidewire is, passed into the pancreatic duct; stones if present are removed from the duct; 5 French pancreatic stents are placed which is removed in 6-8 weeks. Confirmation of the resolution of pseudocyst is done by follow-up CT. This procedure is suitable only in communicating pseudocyst; it is safer and effective.
- Transmural endoscopic or EUS-guided stent placement to the pseudocyst; guided needle aspiration is done initially on the visible bulge; then an endoscopic stent is placed to allow internal drainage; stent is removed after 8 weeks endoscopically. The recurrence rate is high; necrosectomy is not possible.
- Percutaneous drainage under USG guidance-lt is technically easier; catheter drainage is done after placing the catheter under guidance in large pseudocyst; high recurrence, infection, displacement, and blockage of the catheter are common.
- Simple US-guided aspiration has got a high recurrence and failure rate; so it is not practiced routinely.
- Surgical drainage-It is either open or laparoscopic method.
Indications for surgery/intervention
A person should take surgery as a treatment if there are given below indications seen in the person:
- Size more than 6 cm
- Formed pseudocyst
- Infected pancreatic cyst
- Cyst persisting after 6 weeks/progressive cyst
- Multiple cysts/cyst due to trauma
- Communicating cysts/cyst with severe pain
- Thick-walled pseudocyst
Surgery
- Cystogastrostomy: At laparotomy, the anterior wall and posterior wall of the stomach is opened. The brownish fluid is aspirated. The thick capsule of pseudocyst is opened. All fluid with necrotic material is sucked. Fluid should be sent for cytology, culture, and sensitivity and amylase estimation. pancreatic cyst wall always should be biopsied. The cyst cavity should be washed with normal saline after breaking septae. Pseudocapsule is anastomosed to the posterior wall of the stomach-Jurasz operation.
Other procedures
Beside surgery here are other procedures which can help in treatment of pancreatic pseudocyst
- Cystojejunostomy is done in a large cyst, a recurrent cyst.
- If infected, cystogastrostomy with external drainage is done using Malecot’s catheter (Smith operation).
- Laparoscopic cystogastrostomy is becoming popular, effective, and less invasive.
- additionally, with cystojejunostomy, pancreaticojejunostomy should be done if there is ductal stricture and addendum and communication with pseudocyst.
- Distal pancreatectomy with pseudocyst removal if the cyst is in the distal part.
Complications of pseudocyst
Complications may arise in people suffering from a pseudocyst. So, the complication of pseudocyst are given below:
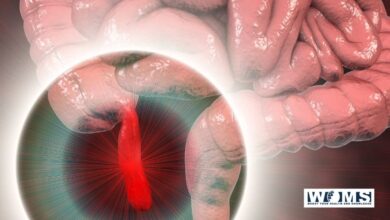
- Rupture—3%—into bowel or peritoneum
- Infection, commonest—-20%, abscess
- Bleeding from the splenic vessels—7%
- Cholangitis
- Duodenal obstruction
- Portal/splenic vein thrombosis and segmental portal hypertension
- Cholestasis due to CBD block
Note:
- Roux-en-Y Cystojejunostomy is better with a lesser recurrence rate than cystogastrostomy.
- Pseudopseudopancreatic cyst: It is a mass in the epigastric region due to pancreatitis formed by bowel, omentum which clinically mimics a pseudocyst of pancreas. But the fluid collection is absent.
- The small cyst can be drained through endoscopy. But debridement is not possible. Bleeding and cyst leakage are other problems.
- CT-guided percutaneous catheter placement is done in critically ill patients, infected pseudocyst, unfit patients, cyst in pelvis/mediastinum. Improper drainage, recurrence, and fistula formation are the problems.
- External drainage is done when the cyst is infected, hemorrhagic or ruptured. The problem with external drainage is the formation of fistula(20%).
- Therapy is decided based on the thickness of the wall of pseudocyst; location of pseudocyst; contents of pseudocyst and ductal status.
- Pseudocysts following trauma and chronic pancreatitis have got lesser chances of spontaneous resolution.
- Pseudocyst of pancreas following biliary pancreatitis has got 4 times more mortality than that of alcoholic pancreatitis,
- Spontaneous resolution rate is 40% for pseudocyst less than 6 weeks; 8% for 6-12 weeks; less than 1% for cyst for more than 12 weeks.
- The presence of significant debris is a contraindication for endoscopic or image-guided drainage.