Leprosy Prevention [Hansen’s disease]
Leprosy (Hansen’s disease)
Medical blogs for students about Leprosy Prevention. An ancient, chronic, progressive bacterial infectious disease caused by
Leprosy is spread between people. This is thought to occur through a cough or contact with fluid from nose of an infected person. Leprosy occur more commonly among those living in poverty. The two types of the disease are based on the number of bacteria present; paucibacillary and multibacillary. These two types are differentiated by the number of poorly pigmented, numb skin patches presents, with paucibacillary having five or fewer and multi bacillary have more than five. The diagnosis is confirmed by finding acid-fast bacilli in biopsy of skin, detecting the DNA using polymerase chain reaction.
Leprosy has affected humanity for thousands of years. The disease takes its name from the Greek word while the term Hansen’s Disease is named after the Norwegian physician Gerhard Amrauer Hansen. World leprosy day was started in 1954 to draw awareness to those affected leprosy.
Bacteriology
- They are straight or slightly curved rod-like bacilli.
- It measures about (3*0.5micrometer)
- Weakly Gram+ve and stained by
ziehi -Neelsen - M.leprae an obligate intracellular acid fast bacillus.
- It has never been grown in artificial media.
- It grows in nine-banded armadillo.
- Replicate very slow(every 12 days once).
- Has an affinity for macrophage and Schwann cell.
- It grows best at 27-30 degree centigrade, hence its predilection for cooler areas of the body.
- Skin, peripheral nerves, anterior chamber of the eye, upper respiratory tract and testes.
Symptoms
The main symptoms of leprosy include:
- Muscle weakness
- Numbness in the hands, leg, arm and feet
- Skin lesions
- The skin lesions results in decreased sensations to touch, pain and temperature. They don’t heal after several weeks. They are lighter than the normal skin of your tone or they may be reddened from inflammation.
Mode of transmission
- The exact route of transmission is not fully known.
- It is believed that leprosy is spread via Nasal discharge (droplets Infections)
- Every 1 cc of nasal secretion contains 1-2 millions leprae bacilli.
Other mode transmission
- Contact through skin (rare).
- Arthropod-born infection (rare),
- Through placenta and milk.
Leprosy in not an STD or directly inherited.
Is leprosy curable?
According to WHO (world health organization)about more than 1,80,000 people are infected with leprosy worldwide, most of them are Africa and Asia. In Asia, leprosy is greatly reported in India as it is no more stigma. If people get diagnosed with leprosy they feel little bit shock that it is not curable.
By leprosy is curable which maximum of people are unaware of it. Please do read below for the leprosy prevention and its treatment.
Leprosy prevention and control
The best way to prevent leprosy is to avoid long term, close contact with an untreated person who has the infection.
The previous strategy of centralized leprosy control campaigns has been superseded by integrated programmes, with primary health-care workers in many countries now responsible for case detection and provision of MDT. it is not yet clear how successful this will be, especially in the time-consuming area of disability prevention.
BCG vaccination has been demonstrated to give good but variable protection against
Epidemiology
- Leprosy is disease of developing countries, but affect all races.
- Registered access of the leprosy has been falling from 5.4 million worldwide in 1985 to below one million in 1998.
- 80% of worldwide cases are found in five countries, namely India, Myanmar, Indonesia, Brazil and Nigeria.
- The incubation period ranges from 2-5 years.
- Males appear to be twice as common than females.
- Bi modal age(10-14 years and 35-44 years)
- Children are more susceptible to this disease.
- Genetic factors, e.g., HLA markers may determine the type of leprosy which patients develop.
Host
Age: Diseases of active age (5 to 40) years
Sex: Incidence is higher in male, but the female is more exposed to risk (delivery, abortion and puerperal tetanus)
Occupation: Agriculture worker-contact with soil
Rural: Urban differences-lower in urban
Immunity: None is immune unless protected by previous immunization or for a few weeks after birth (as maternal A transfer to the baby)
Predisposing or risk factors
- Residing in an endemic area.
- Having a blood relative with leprosy.
- Poverty (malnutrition).
- Contact with affected armadillo.
Classifications and clinical presentations
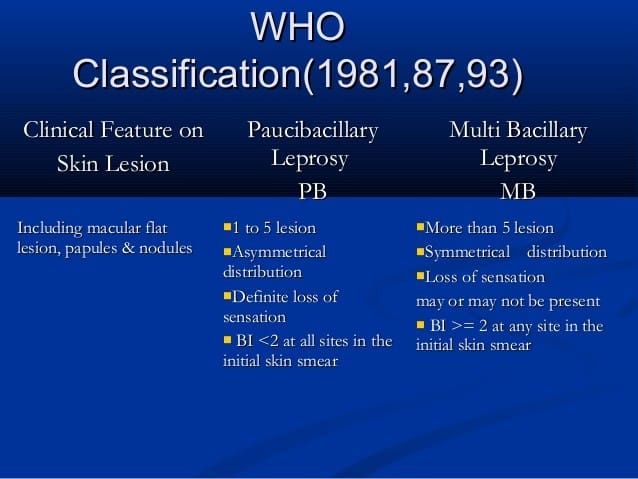
Indeterminate Leprosy (IL)
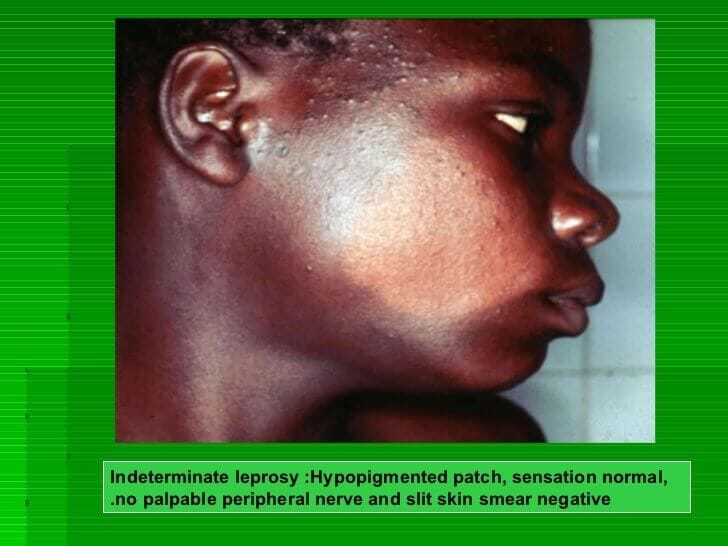
- . Usually a single (multiple) Macaulay/patches.
- Hypo pigmented or faintly erythematous.
- Sensation normal but sometimes impaired.
- The peripheral nerves normal.
- Slit skin smear negative.
Tuberculoid Leprosy (TL)

- Usually single, but may be few(<5).
- Hypopigemented/erythematous plaque.
- Varying in size from few MM to several CM.
- Well defined borders.
- Sensation markedly impaired.
- Enlarged peripheral nerves.
- Slit skin smear negative.
Borderline leprosy (BL)

- Few/many asymmetrical patches.
- Partly well defined borders.
- Sensory impairments range from slight to marked.
- Slit skin smear usually positive.
- Peripheral nerves asymmetrically enlarged.
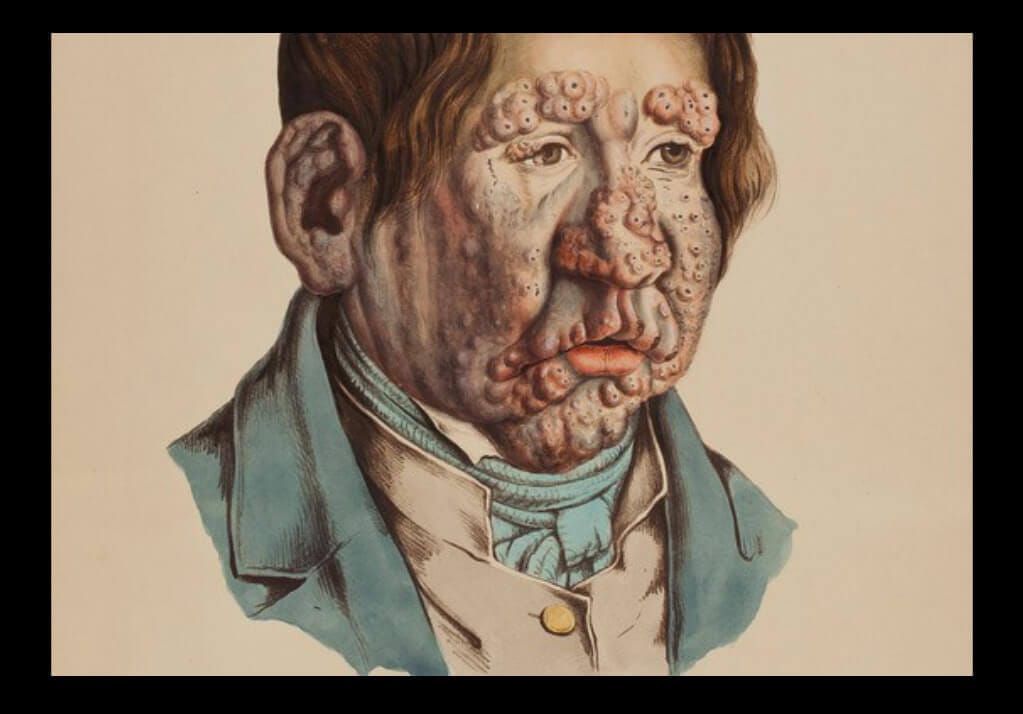
Lepromatous Leprosy (LL)

- Very numerous ill defined lesions. (Macula’s, patches, papules, and nodules).
- Symmetrically disturbed all over the body.
- Loss of eyebrows and eyelashes.
- Leonine faces.
- No sensory impairments in lesions.
- Peripheral nerves symmetrically enlarged.
- Slit skin smear always positive.
Diagnosis of leprosy
- Clinical examinations.
- Slit skin smear.
- Skin Biopsy
1. CLINICAL EXAMINATIONS
What are the cardinal skin signs of leprosy?
- Hypopigmented or erythematous patch/plaque.
- Complete/[Arial loss of sensations.
- Thickening of peripheral nerves.
2. Slit Skin Smear
- Simple and valuable test.
- It is needed for diagnosis.
- Monitor the progress of the treatment.
Slit Skin Smear (Method)
- Pinch the site tight.
- Scrape and collect material
- Smear on a slide.
- Air dry and fix
- Stain (Z-N method)
Slit Skin Smear (Site)
- Ear lobule
- Forehead
- Gluteal region
- Active edge patch
Drugs used in leprosy treatment
What are three commonly used drugs?
- Dapsone
- Clofazimine.
The combinations of these 3 drugs is known as multi drug therapy (MDT)
Rifampicine is highly bactericidal 99.999% of bacilli will be killed within 3 monthly doses.
Dapsone and calofazimine are weekly bactericidal, but in combination will kill 99.999% of bacilli within 3 months.
MDT (Chemotherapy) renders leprosy patients non-infectious.
Treatments
Leprosy is a curable disease. Leprosy treatment is simple, available free and drugs are supplied in packs that contain correct dose for 4 weeks. All you have to do is to decide which course of treatment the patient needs and make sure that he takes it regularly. Best
Recommended by WHO-(adult dose schedule)
For Multi Bacillary Leprosy (person having 6 or more lesions and/ or more than one nerve involvement)
For 12 months, Complete within 18 months with-
- Rifampicin-600mg once monthly, given under supervision
- Dapsone-100mg daily, self-administered
- Clofazimine-300mg once monthly supervised; and 50mg daily self-administered
For Paucibacillary (person having 1-5 lesions and/or only one nerve involvement)
For 6 months, complete within 9 months with
- Rifampicin-600mg once a month, given under supervision
- Dapsone-100mg daily(1-2mg/kg body weight), self administered
Complications of leprosy Prevention
- Reactions
- Complications of peripheral nerves.
- Problems of eyes.
- Complications of bones.
Types of Leprae reactions
Type one Leprae reaction (Reversal reaction)
- Seen in BT, BB and BL
- Sudden onset,
- Erythematous and edematous changes in older lesions
- Appearing of new lesions
- Tenderness and swelling of peripheral nerves
Treatment of type one Reaction:
- Continue MDT
- NSAID
- Type 2 two leprae reactions (ENL)
- Acute onset of constitutional symptoms
- Appearance of ENL-like skin lesions
- Visceral manifestations includes:- Iridocyclitis, hepato-spleenomegaly, epididmoorchitis, nephritis, pleuritis, lymphadenitis and neuritis.
Treatment of type two Reaction:
- Continue MDT
- NSAID
Summary
Leprosy is a chronic granulomatous disease affecting skin and nerves and caused by the Mycobacterium Leprae, a slow-growing Mycobacterium that cannot be cultured in vitro. the clinical manifestations are determined by the degree of the patient’s cell-mediated immunity (CMI) towards Mycobacterium leprae.
The best way for leprosy prevention is to avoid long term, close contact with an untreated person who has the infection. BCG vaccination has been demonstrated to give good but variable protection against leprosy; adding killed M.leprae to BCG does not enhance protection.