Heart failure guidelines for treatment
overview I classification I sign and symptoms I complications I Pathophysiologic changes in heart failure I Investigations I Treatments
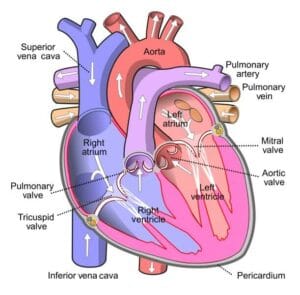
This is a topic on Heart failure guidelines for treatment. Heart failure is a clinical condition when the heart cannot maintain an adequate cardiac output or can do so only at the expense of elevated filling pressure.
In mild to moderate forms of heart failure, symptoms occur when the metabolic demand increases during exercise or some other form of stress. In severe heart failure, symptoms may be present at rest. In clinical practice, heart failure may be diagnosed when a patient with significant heart disease develops the signs or symptoms of low cardiac output, pulmonary congestion or systematic venous congestion at rest or on exercise.
Classification of heart failure | Heart failure guidelines
A) According to the ventricular involvement
1) Left heart failure: Common causes are acute myocardial infarction (MI), hypertension, aortic valvular disease.
2) Right-sided heart failure: causes of isolated right heart failure include
- Chronic lung disease (cor pulmonale)
- Pulmonary embolism and
- Pulmonary valvular stenosis
3) Biventricular heart failure
B) Forward and backward heart failure
- Forward failure: the predominant problem is an inadequate cardiac output.
- Backward failure: patients may have a normal or near-normal cardiac output with marked salt and water retention causing pulmonary and systematic venous congestion.
C) Diastolic and systolic dysfunction
- Systolic dysfunction: heart failure may develop as a result of impaired myocardial contraction.
- Diastolic dysfunction: heart failure due to poor ventricular filling and high filling pressure caused by abnormal ventricular relaxation.
D) High-output failure: conditions that are associated with a very high cardiac output
(e.g. a large arteriovenous shunt. Beriberi, severe anemia or thyrotoxicosis) can occasionally cause heart failure.
E) Acute and chronic heart failure:
- Acute heart failure: as in myocardial infarction
- Chronic heart failure: as in progressive valvular heart disease.
New York Heart Association (NYHA) classification:
Before going for heart failure guidelines treatment, it is important to have an idea about NYHA classification which are shown below:
| Class | Criteria |
| Class I | No limitation. Normal physical exercise does not cause fatigue, dyspnoeas, or palpations. |
| Class II | Mild limitation. comfortable at rest, but normal physical activity produces fatigue, dyspnoeas, or palpations. |
| Class III | Marked limitation. comfortable at rest, but less gentle physical activity produces a marked symptom of heart failure. |
| Class IV | In this class symptoms of heart failure occur at rest and are exacerbated by physical activity. |
Sign and symptoms of heart failure | Heart failure guidelines
- Shortness of breath (dyspnoea)
- Fatigue and weakness
- Swelling (edema) in leg, ankle, and feet
- Rapid or irregular heartbeat
- Persistence cough
- Orthopnoea
- Pro station
- Auscultation of heart: a ‘gallop’ rhythm, with a third heart sound.
- Auscultation of the lungs: bilateral basal crepitations.
Complications of heart failure
Heart failure guidelines for treatment must also care for the complication of it. The guideline should also include the treatment of the complications. So, here are some complications of heart failure
1. Renal failure: caused by poor renal perfusion due to low cardiac output and may be exacerbated by diuretic therapy, ACE inhibitors, and angiotensin receptor blockers.
2. Hypokalaemia: a result of treatment with potassium-losing diuretics or hyperaldosteronism caused by activation of the renin-angiotensin system and impaired aldosterone metabolism due to hepatic congestion.
3. Hyperkalemia: due to the effects of drug treatment, particularly the combination of angiotensin in converting enzymes (ACE) inhibitors and spironolactone (which both promote potassium retention), and renal dysfunction.
4. Hyponatremia: caused by diuretic therapy, inappropriate water retention due to high ADH secretion, or failure of the cell membrane ion pump.
5. Impaired liver function: caused by
- Hepatic venous congestion
- Poor arterial perfusion
6) Thromboembolism: due to the effects of a low cardiac and enforced immobility.
7) Atrial and ventricular arrhythmias
8) Sudden death
Factors that may precipitate heart failure or aggravate heart failure
Factors that may precipitate or aggravate heart failure in patients with pre-existing heart diseases:
- Myocardial ischemia or infarction
- Intercurrent illness (eg. Infection)
- Arrhythmia, eg. Atrial fibrillation
- Inappropriate reduction of therapy
- Administration of a drug with negative inotropic properties (e.g. β-blocker) or fluid-retaining properties (e.g. Non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids).
- Pulmonary embolism
- The condition associated with increased metabolic demand e.g. pregnancy, thyrotoxicosis, anemia
- Intravenous fluid overload, e.g post-operative I/V infusion.
Pathophysiologic changes in heart failure
The pathophysiologic changes of heart failure are:
- Ventricular dilation
- Myocyte hypertrophy
- Increased collagen synthesis
- Altered myosin gene expression
- Altered sarcoplasmic calcium- ATPase density
- Increased ANP secretion
- Sympathetic stimulation
- Peripheral vasoconstriction
Investigations
Investigations must be done in order to confirm heart failure and for heart failure guideline treatment. Here is a list of investigations done for the diagnosis and the confirmation of heart failure:
- ECG: features of MI, ischemia, LVH, etc
- Chest x-ray P/A view: pulmonary edema, cardiomegaly
- Echocardiography
- Blood test: serum creatinine, blood ureas, electrolytes, full blood count, cardiac enzymes, CRP, blood glucose level.
Treatment

Treatment of acute left heart failure/ acute left ventricular failure
- The position of the patient: sitting up (propped up), in order to reduce pulmonary congestion.
- Oxygen: high flow, high concentration.
- Continuous positive airway pressure,
- Nitrates: the patient should be given IV glyceryl trinitrate 10-200 µg/min or buccal glyceryl trinitrate 1-5 mg titrated upwards every 10 minutes until clinical improvement occurs or the systolic blood pressure of the patient falls to 110 mmHg
- Loop diuretic: furosemide 50-100 mg IV.
- Intravenous opiates: may be cautiously used when patients are in extremis (morphine/pethidin=anti-emetic).
- If these measures prove ineffective, inotropic agents may be required to augment cardiac output, particularly in hypotensive patients.
- Insertion of an intra-aortic balloon pump may be beneficial in patients with acute cardiogenic pulmonary edema and shock.
Chronic heart failure
General management
- Education
- Salt and water retention
- Avoidance of smoking and alcohol
- Regular exercise within a limit
Drugs
- Diuretics: loop diuretic and a potassium-sparing diuretic
- ACE inhibitors or ARB
- Neprilysin inhibitors e.g. sacubitril
- Beta-blockers
- Digoxin
- Ivabradine
Non-pharmacological treatments:
- Implantable cardiac defibrillators.
- Resynchronization devices
- Coronary revascularization
- Cardiac transplantation
- Ventricular assisted devices.
Biventricular failure/ congestive cardiac failure (CCF)
A) General measures
- Education: in this, explanation of the nature of the disease, treatment, and self-help strategies.
- Diet: good general nutrition and reduction of the obese. Avoidance of high-salts food and added salt.
- Alcohol: moderate or eliminate alcohol consumption.
- Stop smoking.
- Exercise: regular moderate aerobic exercise within limits of symptoms.
- Vaccination: influenza and pneumococcal vaccination should be considered.
B) Drug therapy:
- Diuretics: these are usually first-line treatments.
- Vasodilators: arterial dilator (eg. Hydralazine) reduce afterload.
- Angiotensin-converting enzyme (ACE) inhibitors
- Angiotensin receptor blockers: Examples include losartan 50-100 mg once daily, candesartan 4-16 mg daily or valsartan 40-160 mg daily.
- Beta-adrenoceptor antagonists (blockers): bisoprolol started at a dose of 1.25 mg daily, and increased gradually over a 12-week period to a target maintenance dose of 10 mg daily.
- Digoxin
- Amiodarone: effective in the treatment of symptomatic arrhythmia.
- Neprilysin inhibitors e.g. sacubitril
- Ivabradine
c) Implantable cardiac defribillators
d) Resynchronization devices
e) Revascularization:
- Coronary artery bypass surgery
- Percutaneous coronary intervention
F) Heart transplantation (intractable heart failure):
- Coronary artery disease
- Dilated cardiomyopathy
G) Ventricular assisted devices
Summary
Do you know heart failure is a lifelong condition affecting 6 million adults in the USA? If you talk about India, about 54.5 million people were affected by heart failure in 2016. For treatment, it’s very important to follow heart failure guidelines for treatment which is discussed above. If you do have any questions regarding heart failure treatment guidelines, feel free to comment below.