What are the appendicitis symptoms?
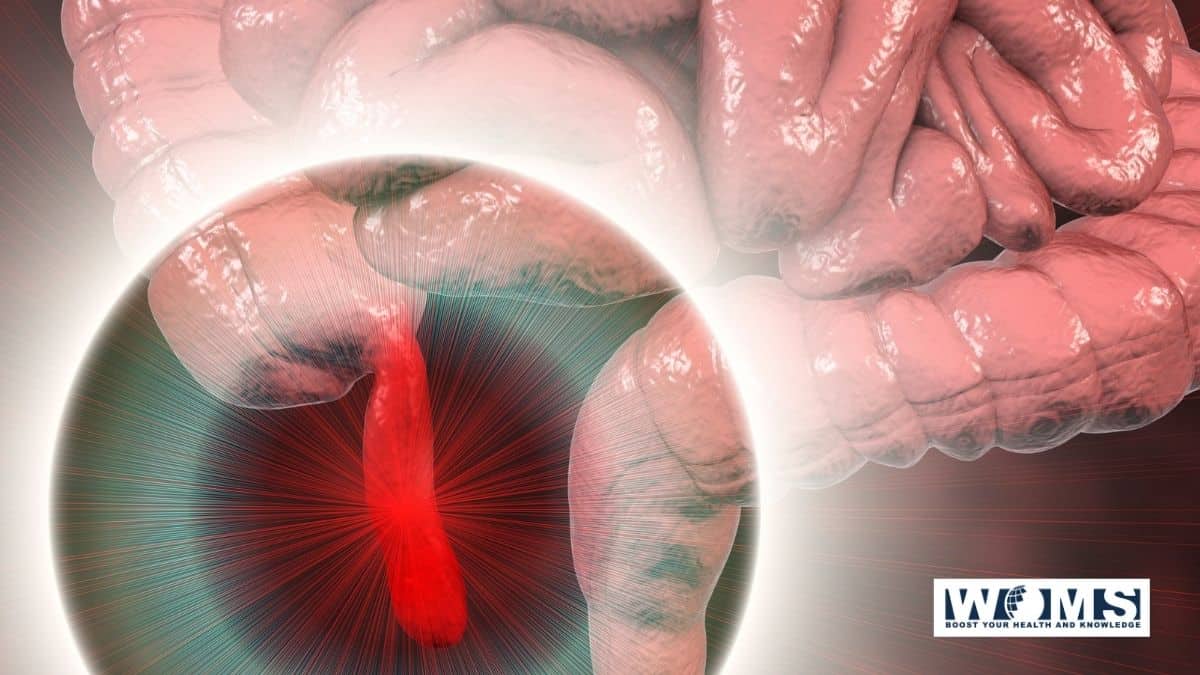
Appendicitis is a condition that is caused by the inflammation of the appendix.
The appendix is an organ that is present on the lower right side of the abdomen. In the case of appendicitis, pain can be felt in the lower right side of the abdomen.
Appendicitis symptoms and signs
The partial inflammation of the peritoneum, in the iliac fossa, is sometimes set up by disease in Appendix Caeci. The classic appendicitis symptoms are discussed below in the principle article.
The appendix having been perforated by ulcerations, occasioned by the lodgement of the fecal concretions in its cavity, extravasation takes place, and inflame-motion of a more severe and serious kind is originated.
Nature sometimes succeeds in limiting the inflammation to the part right side, but it is at other times diffused over the whole abdomen, and quickly proves fatal.
Etiology of appendicitis
- It is common in young males.
- It is common in white races.
- Fibre-rich diet prevents apendicitis. A less fiber diet increases the chance of appendicitis.
- It is familiar in May, and August-seasonal variation-often called epidemic appendicitis.
- Active infection may cause mucosal edema, inflammation, and that afters get contaminated by bacteria causing appendicitis.
- The family records may be relevant in 30% of appendicitis in children with appendicitis occurring in first-degree relatives.
- Obstruction of the lumen of the appendix resulting in obstructive appendicitis.
-
- Blockage occurs due to—faecoliths, stricture, foreign body, roundworm, or threadworm.
- Adhesions and kinking—carcinoma caecum near the base, ileocaecal Crohn’s disease.
- Distal colonic obstruction.
- Abuse of purgatives.
- Faecolith is the most common cause.
Organisms:
E. Coli (85%), enterococci, (30%), streptococci, Anaerobic streptococci, Cl. Welchii, Bacteroides.
Pseudoappendicitis is appendicitis due to acute ileitis following Yersinia infection. It is often due to Crohn’s disease.
Appendicitis symptoms
The common appendicitis symptoms are enlisted below:
- Sudden right lower quadrant pain
- Sudden pain that impels around your navel and repeatedly shifts to your lower right abdomen.
- Pain that aggravates if you cough, walk or make any jarring movements.
- Nausea and vomiting
- Low-grade fever
- Loss of appetite (anorexia)
- Constipation or diarrhea
The site of your pain may alter, depending on your age and the position of your appendix. When you’re pregnant, the pain may seem to begin from your upper abdomen because your appendix is superior to the normal position during pregnancy.
Clinical signs in appendicitis
- Rovsing’s sign
- Rebound tenderness
- Blumberg’s sign (Release sign)
- Cope’s psoas test
- Obturator test
- Baldwin’s test
- Bastede sign
- Dumphy’s cough tenderness sign (Refer fascinating signs for detail)
- Bapat bed shaking test
- Heel Drop test
Acute appendicitis in infancy
Even though it is rare when it occurs, it has got 80% chances of perforation with high mortality (50%).
Signs of appendicitis in kids
The signs of appendicitis in kids are:
- Severe right lower quadrant pain (dull pain in the lower right abdomen that comes and goes)
- Low-grade fever
- Anorexia (loss of appetite)
- Nausea and vomiting
Acute appendicitis in children:
-
- Here localization is not present, and so peritonitis occurs early.
- It requires early surgery. Dehydration, septicemia are common.
In elderly:
Gangrene and perforation are common. Because of the lax abdominal wall, localization is poor, and so peritonitis sets in early.
In pregnancy:
- Incidence is 1 in 2,000 pregnancies. It is more common in 1st and 2nd trimesters.
- Appendix shifts to the upper abdomen. So pain is higher and more lateral.
- Rebound tenderness and guarding may not be evident.
- TC will be very high with neutrophilia.
- The risk of premature labor is 15%.
- Fetal death in early appendicitis is 5% but becomes 29% once the appendix perforates in pregnancy.
- After six months, maternal mortality increases by ten times than usual and also leads to premature labor.
- Appendicitis is the most common non-gynaecologic surgical emergency during pregnancy. The appendicitis symptoms for gynecological patients are also the same as non-gynecological patients.
- The incidence of perforation is highest in 3rd trimester.
- Surgery is the treatment.
Pathogenesis
- Acute inflammation of the mucous membrane with the secondary disease without obstruction causes acute nonobstructive appendicitis. It may lead to resolution, fibrosis, recurrent appendicitis, or eventual obstructive appendicitis.
- Luminal obstruction by faecolith, lymphoid hyperplasia, pinworm (Oxyuris Vermicularis), other worms, foreign body, carcinoma/Crohn’s disease-mucus, and inflammatory fluid collects inside the lumen–increases intraluminal pressure—leads to blockage of lymphatic and venous drainage–resulting in increased edema of mucosa and wall-causes mucosal ulceration and ischemia —bacterial translocation —bacterial spread through the submucosa and muscular Propria –acute obstructive appendicitis—thrombosis of the appendicular artery–ischaemic necrosis of full thickness of the wall of the appendix–gangrene of the appendix—perforation at the tip or the base–peritonitis.
- After perforation– localization by greater omentum and dilated ileum occurs—with suppuration and pus inside forming an appendicular abscess.
- In severe acute appendicitis, —localization can occur by omentum and dilated ileum without pus inside—forming an appendicular mass.
- Acute appendicitis with obstruction at the opening of the lumen—inflammation rarely subsides—mucus collects inside the lumen of the appendix resulting in its enlargement—Mucocele of the appendix.
Types
Acute nonobstructive appendicitis (catarrhal) (mucosal appendicitis):
Inflammation of mucous membrane occurs with redness, edema, and hemorrhages which may go for following courses:
- Resolution
- Ulceration
- Fibrosis
- Suppuration
- Recurrent appendicitis
- Gangrene-rare initially in nonobstructive type but later can occur
- Peritonitis.
- Acute obstructive appendicitis: Here, pus collects in the blocked lumen of the appendix, which is blackish, gangrenous, oedematous, and rapidly progresses, leading to perforation either at the tip or the base of the appendix. This leads to peritonitis, the formation of an appendicular abscess or pelvic abscess. Most often, there will be thrombosis of the appendicular artery. The appendicitis symptoms may vary in obstructed cases.
- Recurrent appendicitis: Repeated attacks of nonobstructive appendicitis leads to fibrosis, adhesions causing recurrent appendicitis.
- Subacute appendicitis is a milder form of acute appendicitis.
- Stump appendicitis is retained long stump of the appendix after commonly laparoscopic appendicectomy.
- It is rare before the age of two, common in children and other age groups.
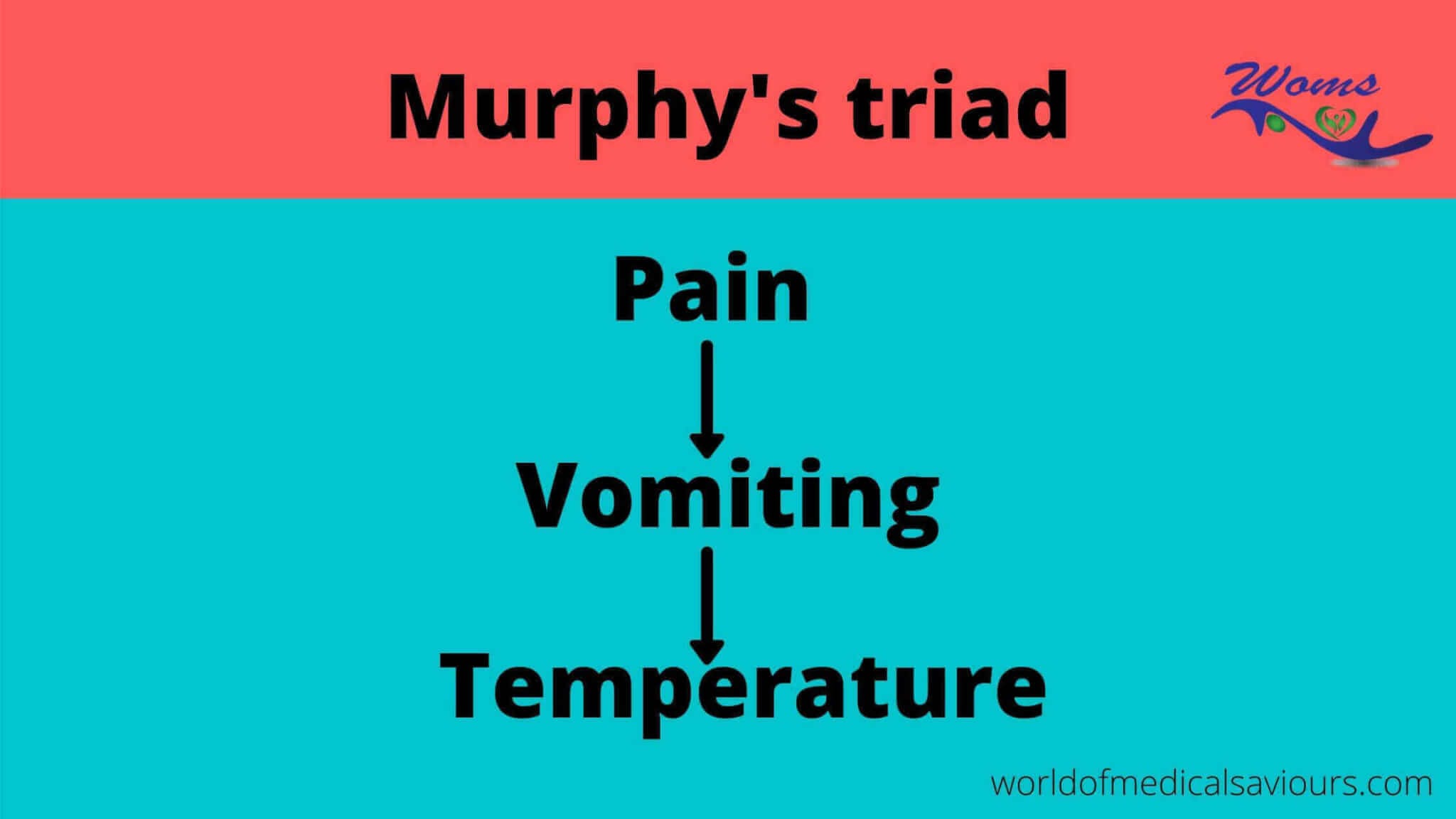
- Pain: It is the earliest symptom. Visceral pain starts around the umbilicus due to distension of the appendix, and later after a few hours, somatic pain occurs in the right iliac fossa due to irritation of the parietal peritoneum inflamed appendix. The pain eventually becomes severe and diffuse, which signifies the spread of infection into the general peritoneal cavity.
- Vomiting: Due to reflex pylorospasm.
Murphy's triad
- Constipation is the usual hallmark, but diarrhea can occur if the appendix is in post ileal or pelvic positions.
- Fever, tachycardia, foetor oris are other features.
- Urinary reiterations: Inflamed appendix may come in touch with bladder and can cause bladder irritation.
- Tenderness and rebound tenderness at McBurney’s is the point in the right iliac fossa (release sign-Blumberg ‘s sign) are typical.
- Rovsing’s sign: On palpating the left iliac fossa, pain occurs in the right iliac fossa, which is due to the shifting of bowel loops, which irritates the parietal peritoneum.
- Hyperextension (in case of retrocausal appendix-Cope’s psoas test) or internal rotation (in case of the pelvic appendix-obturator test) of the right hip causes pain in the right iliac fossa due to irritation of psoas muscle and obturator internus muscle respectively.
- Baldwin’s test is positive in Retrocaecal appendix-when legs are lifted off the bed with the knee extended, the patient complains of pain while pressing over the flanks.
- P/R examination shows tenderness on the right side of the rectum
- Hyperaesthesia in ‘Sherren’s triangle.’ This triangle is assembled by the anterosuperior iliac spine, umbilicus, pubic symphysis.
Differential Diagnosis for Acute Appendicitis
Many conditions mimic acute appendicitis. It differs in children, adults, the elderly, and females.
- They have a perforated duodenal ulcer. In duodenal ulcer perforation, fluid creeps to the bottom along the right paracolic gutter and mimics appendicitis. Upper abdominal pain, obliterated liver dullness, gas under the diaphragm in X-ray, and CT scan differentiate it from acute appendicitis.
- Acute cholecystitis: Pain in the right upper abdomen, fever, jaundice, upper abdominal guarding are the features of acute cholecystitis. US; HIDA scan, LFT will differentiate it from acute appendicitis.
- Acute pancreatitis: Pain in epigastrium, radiating to back, raised serum amylase and lipase, CT abdomen with a history of alcohol intake often are diagnostic.
- Right ureteric colic: Pain is colicky in nature, which often refers to genitalia. Haematuria, urinary symptoms are common. It mimics Retrocaecal/pelvic acute appendicitis. Often in ureteric stone, the abdomen is soft and non-tender. CT is an important way to differentiate.
- Acute typhlitis: Inflammation of the caecum is called typhlitis. Often it is difficult to differentiate it from acute appendicitis. Intravenous/oral metronidazole completely controls the disease.
- Acute bacterial enterocolitis: It presents with pain abdomen, diarrhea, toxemia, dehydration. Often it is difficult to differentiate from acute appendicitis.
- Right-sided acute pyelonephritis: Here, there will be pain and tenderness in the loin. Urine analysis, US are diagnostic. Often DTPA scan may be needed.
- Crohn’s disease presenting with acute symptoms will have similar features of acute appendicitis.
- Pelvic inflammatory disease, like salpingo-oophoritis, mimics acute appendicitis. Twisted/hemorrhagic/ruptured ovarian cyst/ruptured ectopic gestation/endometriosis/Tubo-ovarian abscess mimics acute appendicitis. US laparoscopy helps to differentiate it from others. Mittelschmerz is lower abdominal pain due to the rupture of follicular cyst during midcycle. It subsides on its own. There are no systemic features.
- Meckel’s diverticulitis presents clinically like acute appendicitis. It is not possible to differentiate between two clinically.
- Intussusception mimics acute appendicitis in children. ISS is common before the age of 2 years. Acute appendicitis is rare before the age of 2 years. Palpable mass, features of intestinal obstruction, barium enema X-ray, US are useful methods to differentiate.
- Worm infestation (roundworm bolus/ball): It often presents as pain in the right iliac fossa. Features of intestinal obstruction are common here.
- Right-sided lobar pneumonia and pleurisy are often not easy to differentiate from acute appendicitis. Pleural rub, change in breath sounds, chest X-ray can identify pneumonia.
- Testicular torsion/acute severe orchitis often looks like acute appendicitis. Referred pain in the iliac fossa, and if scrotum is not palpated clinically these conditions are mistaken for acute appendicitis. These problems are much more obvious if the testis is undescended
- Sigmoid diverticulitis in the elderly with a loop lying towards the right side may present as pain in the right iliac fossa.
- Carcinoma caecum may present with features of acute appendicitis without any earlier typical features.
- Ruptured aortic aneurysm, acute intestinal obstruction, mesenteric ischemia may present as acute appendicitis.
- Rare conditions like preherpetic pain of the right 10th and 11th dorsal nerves may mimic acute appendicitis. Guarding and rigidity will not be present. There will be significant hyperaesthesia.
- Tabetic crisis, tuberculosis of the spine, secondaries in the spine, multiple myeloma, osteoporotic pain often can mimic acute appendicitis.
- Acute crisis of porphyria and diabetes mellitus mimic acute appendicitis with severe abdominal pain.
Differential diagnosis
- Perforated peptic ulcer
- Ruptured or twisted ovarian cyst
- Acute cholecystitis
- Right ureteric colic
- Enterocolitis
- Right acute pyelonephritis
- Mesenteric lymphadenitis
- Lobar pneumonia
- Crohn’s disease
- Acute pancreatitis
- Meckel’s diverticulitis
- Acute crisis of porphyria
- Salpingitis
- Diabetic abdomen
- Ectopic gestation—ruptured
- Typhlitis
Differential diagnosis in children
- Meckel’s diverticulitis
- Acute colitis
- Acute iliac lymphadenitis
- Intussusception
- Roundworm colic
- Lobar pneumonia
Differential diagnosis in females
- Ruptured ectopic gestation
- Mittelschmerz rupture of the ovarian follicle during the mid-menstrual period
- Ovarian cyst torsion
- Salpingo-oophoritis
Differential diagnosis in the elderly
- Acute diverticulitis
- Carcinoma caecum—acute features
- Mesenteric ischemia
- Intestinal obstruction
- Aortic aneurysm leak
- Crohn’s disease
Sequelae of acute appendicitis
- Resorption
- Relapse and recurrent appendicitis
- Appendicular mass
- Appendicular abscess
- Perforation—has got 20% mortality
- Peritonitis, septicemia
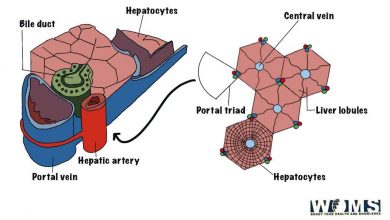
- Portal pyemia
- Intestinal obstruction due to obstructive ileus, inflammatory adhesion, the formation of the band between appendix and omentum or between the appendix and small bowel
Investigations
- The total leucocyte count is increased.
- Ultrasound is done to rule out other conditions like ureteric stone, pancreatitis, ovarian cyst, ectopic pregnancy, and also to confirm appendicular mass or abscess.
- Laparoscopy is the most useful method.
Sonographic criteria for appendicitis (85% Specificity)
- Noncompressible appendix of size > 6 mm AP diameter, hyperechoic thickened appendix wall > 2 mm—target sign.
- Appendicolith.
- Interruption of submucosal continuity.
- Periappendicular fluid.
- Kalam modified Alvarado scoring (1994), where the shift to the left is removed.
- Tzamakis scoring system 2005-lower abdominal tenderness-4; rebound tenderness-3; total count> 12,000/cm-2; USG features-6.
- RIPASA scoring system (2010)-with parameters.
- Anderson scoring system-8 parameters.
Early symptoms of appendicitis in children
You can see for these symptoms to know about the early symptoms of appendicitis in children.
- The child might be having a mild fever.
- There is a pain in the belly and it might be like a stomach ache but in the case of appendicitis the pain worsens and the pain radiates toward the lower right side of the abdomen.
- Appetite in children seems to be lost
- Feeling nauseous and throwing up
- Presence of a swollen belly.
Treatment
Surgery-Appendectomy
- Read all the detail about Appendectomy
- Also, read the prevention of appendicitis
General FAQS
Do appendicitis symptoms come and go?
If it is the case of acute appendicitis then the symptoms can come and remain for some time and then disappear. While if it is acute appendicitis then the symptoms appear and become intense and require treatment immediately.
How to know it is appendicitis or not?
If you have sudden pain in the lower right side of the abdomen then you should look out for the doctor. If there is a pain in the navel but the pain shifts to the lower right side of the abdomen then it might be appendicitis
How long can you have appendicitis symptoms before it bursts?
Not all patients will have the same appendicitis symptoms, but you must visit a surgeon as soon as possible. According to Johns Hopkins Medicine, the vermiform appendix can burst as quickly as 48 to 74 hours after the aggression of appendicitis symptoms.
Where is appendix pain?
The appendix pain is mainly right lower quadrant pain (dull pain in the lower right abdomen that comes and goes) but it starts from the middle of the abdomen mainly at or near the umbilicus. Within a few hours the pain main shift to right lower quadrant (right iliac region). This is the place where the appendix is usually located. The pain became severe when we perform rebound tenderness, or during coughing or walking.