Full details about Anatomy of the heart and it’s structure
Anatomy of the heart
Let’s start with the basic anatomy of the heart. The heart is a conical vaulted muscular organ situated in the middle mediastinum. It is confined within the pericardium. It pumps blood to disparate parts of the body to meet their nutritive requirements. The Greek name for the heart is cardia from which we have the attributive cardia. The Latin name for the heart is cor from which we have the adjective coronary.
The heart is placed obliquely behind the body of the sternum and adjoining parts of the costal cartilages so that one-third of it lies to the right and two-thirds to the left of the median plane. The direction of blood flow, from atria to ventricles is downwards forwards and to the left.
The heart measures about 12×9 cm and weighs about 330g in males and 250 g in females. The anatomy of the heart consists of the external features, blood supply, venous supply, and lymphatic drainage, a development which is discussed in the main article.
External Features
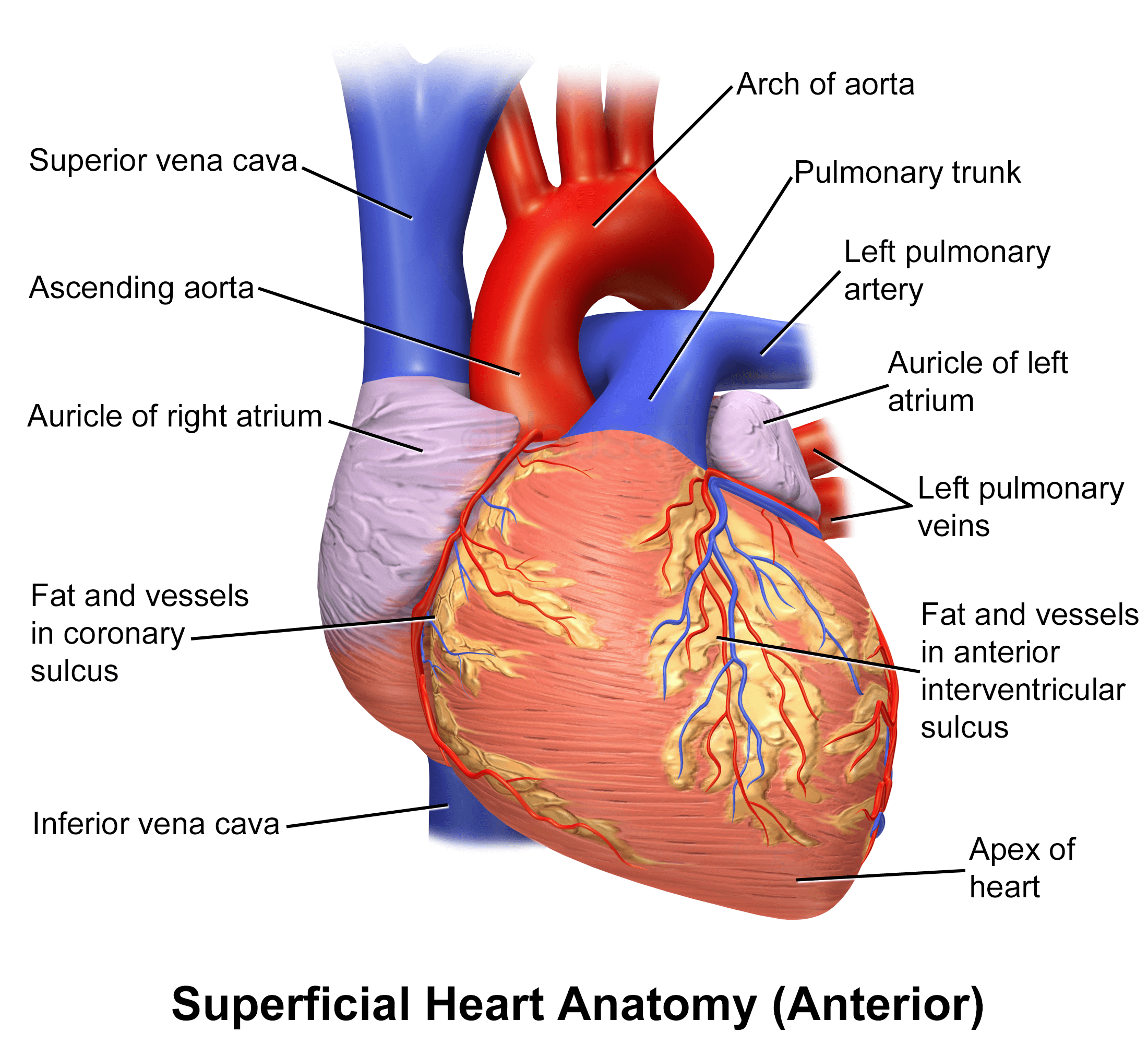
In the title ‘Anatomy of the heart’ let’s learn about the external features of the heart. The human heart has four chambers. These are the right and left atria and the right and left ventricles.
The atria (Latin chamber) lie above and behind the ventricles. On the surface of the heart, they are separated from the ventricles by an atrioventricular groove. The ventricles are separated from each other by an interventricular groove, which is subdivided into anterior and posterior parts.
The heart has
- An apex directed downwards, forwards, and to the left,
- A base (posterior surface) directed backward; and
- Anterior/sternocostal
- Inferior and
- Left lateral surfaces.
The surfaces are demarcated by upper, inferior, right, and left borders.
The above points are the anatomical description of the heart. you must have good knowledge about the anatomical description of the heart while studying the anatomy of the heart.
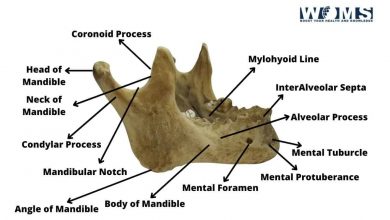
Grooves or sulci
The atria are separated from ventricles by a circular atrioventricular or coronary sulcus. It is divided into anterior and posterior parts. The anterior part consists of right and left halves. The right half is oblique between the right auricle and right ventricle, loading the right coronary artery. The left part is small between the left auricle and left ventricle, and lodges the circumflex branch of the left coronary.
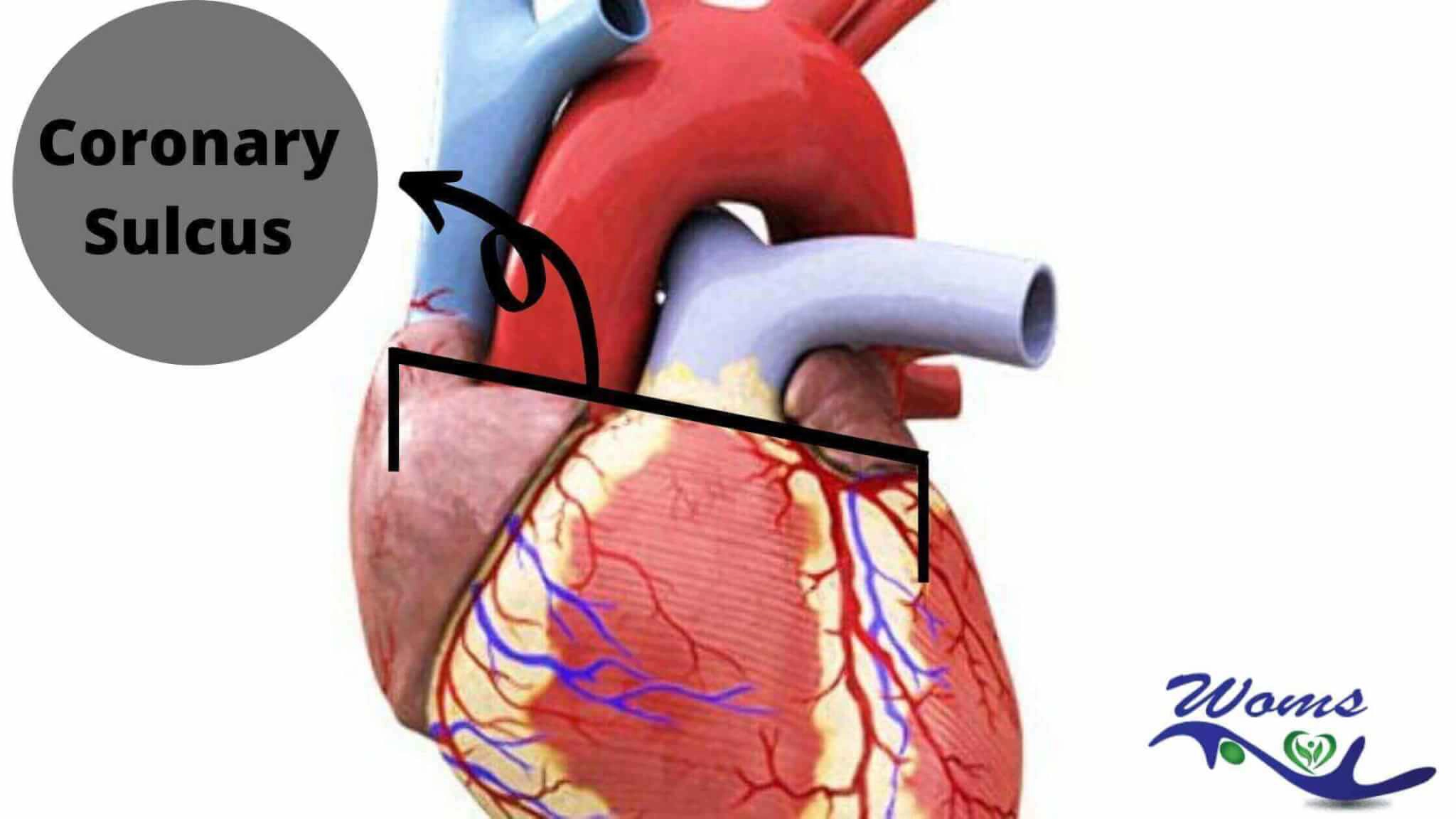
The above image gives a basic idea about the coronary sulcus. It’s really important for the MBBS or BDS student when he/she studies or faces a viva examination on the topic of the anatomy of the heart.
The coronary sulcus is overlapped anteriorly by the ascending aorta and the pulmonary trunk. The interatrial groove is faintly visible posteriorly, while the anteriorly interventricular groove is nearer to the left margin of the heart. It’s run downward and to the left.
The lower end of the groove separates the apex from the rest of the inferior border of the heart. The posterior interventricular groove is situated on the diaphragmatic or inferior surface of the heart. It is nearer to the right margin of this surface. The two interventricular grooves meet at the inferior border near the apex.
The crux of the heart is the point where the posterior interventricular sulcus Mets the coronary sulcus.
The apex of the heart
The apex of the heart is formed entirely by the left ventricle. It is directed downwards, forwards, and to the left and is overlapped by the anterior border of the left lung.
It is situated in the left fifth intercostal space 9cm lateral to the midsternal line just medial to the midclavicular line. The situation of the apex of the heart is really important in the anatomy of the heart. In the living subject, pulsations may be seen and felt over the region.
In children below 2 years, the apex is suited in the left fourth intercostal space in the midclavicular line.
The base of the heart
The base of the heart is also called the posterior surface. it is formed mainly by the left atrium and by a small part of the right atrium.
In relation to the base one can see the opening of the four pulmonary veins which opens into the left atrium; and of superior and inferior venae cavae (Latin, empty vein) which open into the right atrium. It is related to thoracic five to thoracic eight vertebrae in the lying posture and descends by one vertebra in the erect posture. It is separated from a vertebral column by the pericardium, the right pulmonary veins, the esophagus, and the aorta.
Borders of the heart
To have a better idea about the structure of the anatomy of the heart, you must go deep through the borders of the heart.
- The upper border is slightly oblique and is formed by two atria, chiefly the left atrium.
- The right border is more or less vertical and is formed by the right atrium. It extends from superior vena cava to inferior vena cava (IVC).
- The inferior border is nearly horizontal and is formed mainly by the right ventricle. A small part of it near the apex is formed by the left ventricle. It extends from IVC to the apex.
- The left border is oblique and curved. It is formed mainly by the left ventricle, and partly by the left auricle It separates the anterior and left surfaces of the heart and also It extends from the apex to the left auricle.
Surfaces of the heart
The anterior or sternocostal surfaces are formed mainly by the right atrium and right ventricle, and partly by the left ventricle and left auricle.
The left atrium is not seen on the anterior surface as it is covered by the aorta and pulmonary trunk. Most of the sternocostal surface is covered by the lungs, but a part of it that lies behind the cardiac notch of the left lung is uncovered. The uncovered area is dull on percussion. Clinically it is referred to as the area of superficial cardiac dullness.
The inferior or diaphragmatic surface rests on the central tendon of the diaphragm. It is formed in its left two-thirds by the left ventricle, and in its right one-third by the right ventricle. It is transversed by the posterior interventricular groove and is directed downwards.
The left surface is formed mostly by the left ventricle, the upper end by the left ventricle, and the upper end by the left auricle. In its upper part, the surface is crossed by the coronary sulcus. It is related to the left phrenic nerve, the left pericardiacophrenic vessels, and the pericardium.
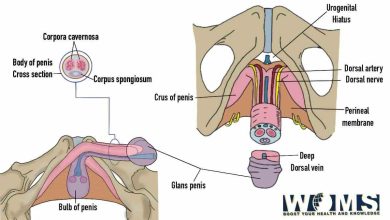
Structures of the heart
Now let’s learn about the structure of anatomy of the heart. The structure of the human heart mainly deals with the valves of the heart.
Valves
The valves of the heart perpetuate the unidirectional flow of the blood and prevent its regurgitation in the opposite direction. There are two pairs of valves in the heart, a pair of atrioventricular valves and a pair of semilunar valves.
The right atrioventricular valve is known as the tricuspid valve because it has three cusps. The left atrioventricular valve is known as the bicuspid valve because it has two cusps. It is also called the mitral valve. The semilunar valves include the aortic and pulmonary valves, each having three semilunar cusps. The cusps are folds of the endocardium, strengthened by an intervening layer of fibrous tissue.
Atrioventricular Valves
- Both valves are made up of the following com
- A fibrous ring to which the cusps are attached
- The cusps are oblate and projected into the ventricular cavity. Each cusp has an attached and a free margin and an atrial and a ventricular surface are rough and irregular due to the attachment of chordate tendinae. The valves are closed during ventricular systole (Greek contraction) by apposition of the atrial surfaces near the serrated margins (Fig. 18.15).
- The chordae tendinae connect the free margins and ventricular surfaces of the cusps to the apices of the papillary muscles. They prevent eversion of the free margins and limit the amount of ballooning of the cusps towards the cavity of the atrium.
- The atrioventricular valves are kept competent by active contraction of the papillary muscles, which pull on the chordae tendinae during ventricular Each papillary muscle is connected to the contiguous halves of two cusps.
2. Blood vessels are present only in the fibrous ring and in the basal one-third of the cusps. Nutrition to the central two-thirds of the cusps is borrowed directly from the blood in the cavity of the heart.
3. The tricuspid valve has three cusps and can admit the tips of three fingers. The three cusps, the anterior, posterior or inferior, and septal aspersion across the three walls of the ventricle. Of the three papillary muscles, the anterior is the arty, the inferior is smaller and aberrant and the septal is represented by a number of small muscular elevations.
4. The mitral or bicuspid valve has two cusps, a blimp anterior or aortic cusp, and a small posterior cusp. It admits the tips of two fingers. The anterior cusp lies betwixt the mitral and aortic orifices. The mitral cusps are lesser and thicker than those of the tricuspid valve.
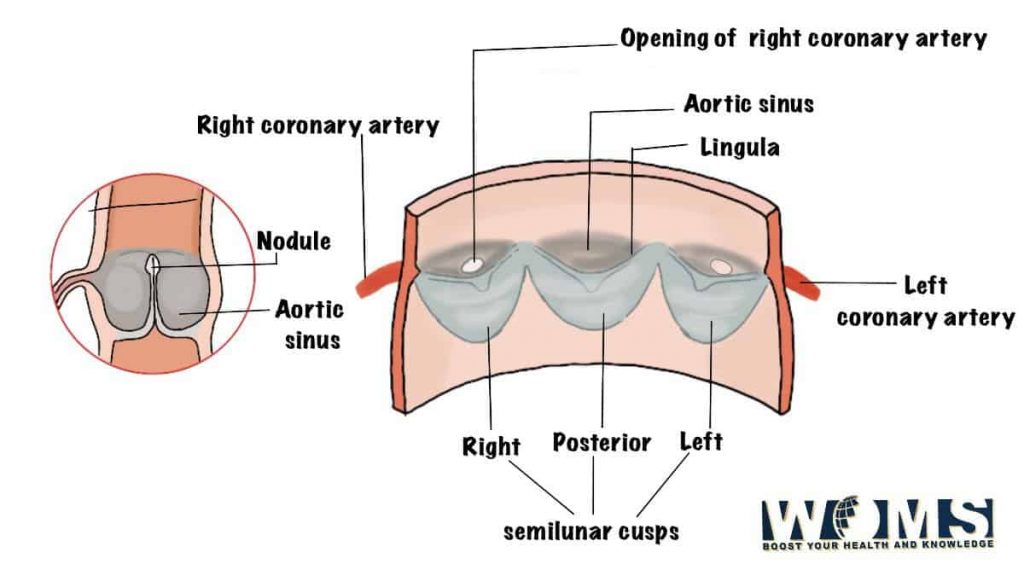
Semilunar Valves
- The aortic and pulmonary valves are called semilunar valves because their cusps are semilunar in shape. Both valves are similar to each other.
- Each valve has three cusps which are attached directly to the vessel wall, there being no fibrous ring. The cusps form small pockets with their mouths directed away from the ventricular cavity. The free margin of each cusp contains a central fibrous nodule from each side of which a thin smooth margin of the lunule extends up to the base of the cusp. These valves are closed during ventricular diastole when each cusp bulges towards the ventricular cavity.
- Opposite the cusps, the vessel walls are slightly dilated to form the aortic and pulmonary sinuses. The coronary arteries arise from the anterior and the left posterior aortic sinuses.
Clinical anatomy of the heart
- The first heart sound originated from the cessation of the atrioventricular valves. The second heart sound is produced by the closure of the semilunar valves.
- Narrowing of the valve orifice due to the fusion of the cusps is known as ‘stenosis’, viz. mitral stenosis, aortic stenosis, etc
- Dilatation of the valve orifice or stiffening of the cusps causes imperfect closure of the valve leading to backflow of blood. This is known as incompetence or regurgitation, e.g. aortic incompetence or aortic regurgitation.
Fibrous Skeleton
The fibrous rings surrounding the atrioventricular and arterial orifices, along with some adjoining masses of fibrous tissue, constitute the fibrous skeleton of the heart. It provides attachment to the cardiac muscle and keeps the cardiac valve competent. The atrioventricular fibrous rings are in the form.
The atria, the ventricles, and the membranous part of the interventricular septum are attached to them. There is no muscular continuity between the atria and ventricles across the rings except for the atrioventricular bundle or bundle of His There is a large mass of fibrous tissue between the atrioventricular rings behind and the aortic ring in front. It is known as the frigonum fibrosum dextrum.
In some mammals like sheep, a small bone the os cordis is present in this mass of fibrous tissue. Another smaller mass of fibrous tissue is present between the aortic and mitral rings. It is known as the trigonum fibrosum sinistrum. The tendon of the infundi-bulum (close to the pulmonary valve) binds the posterior surface of the infundibulum to the aortic ring.
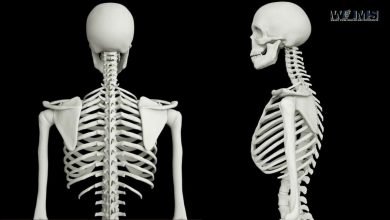
The musculature of the Heart
Cardiac muscle fibres form long loops which are attached to the fibrous skeleton. Upon contraction of the muscular loops, the blood from the cardiac chambers is wrung out like water from a wet cloth. The atrial fibres are arranged in a superficial transverse layer and a deep anteroposterior (vertical) layer.
The ventricular fibres are arranged in superficial and deep layers.
The superficial fibres arise from the skeleton of the heart to undergo a spiral course.
Thorax
(Image Source: BD Chaursaiya)
across the sternocostal surface to reach the apex of the heart, where these fibres form a vortex and continue with the deep layer.
Superficial fibres are:
- Fibres start from the tendon of infundibulum (1) pass across the diaphragmatic surface, curve around the inferior border to reach the sternocostal surface Then these fibres cross the anterior intraventricular groove to reach the apex, where these form a vortex and end in the anterior papillary muscle of left ventricle.
- The fibres arise from the right AV ring and take the same course as (2) but end in the posterior papillary muscle.
- Fibres arise from the left AV ring, lie along the diaphragmatic surface, and cross the posterior interventricular groove to reach the papillary muscles of the right ventricle.
- Deep fibres are ‘S-shaped: These arise from the papillary muscle of one ventricle, turn in an interventricular groove, to end in the papillary muscle of other ventricles. Fibres of the first layer circle RV, cross through the interventricular septum, and end in the papillary muscle of LV. Layers two and three have a decreasing course in RV and increasing course in LV
Arteries supplying the heart
The heart is endowed with two coronary arteries, arising from the ascending aorta. Both arteries run in the coronary sulcus.
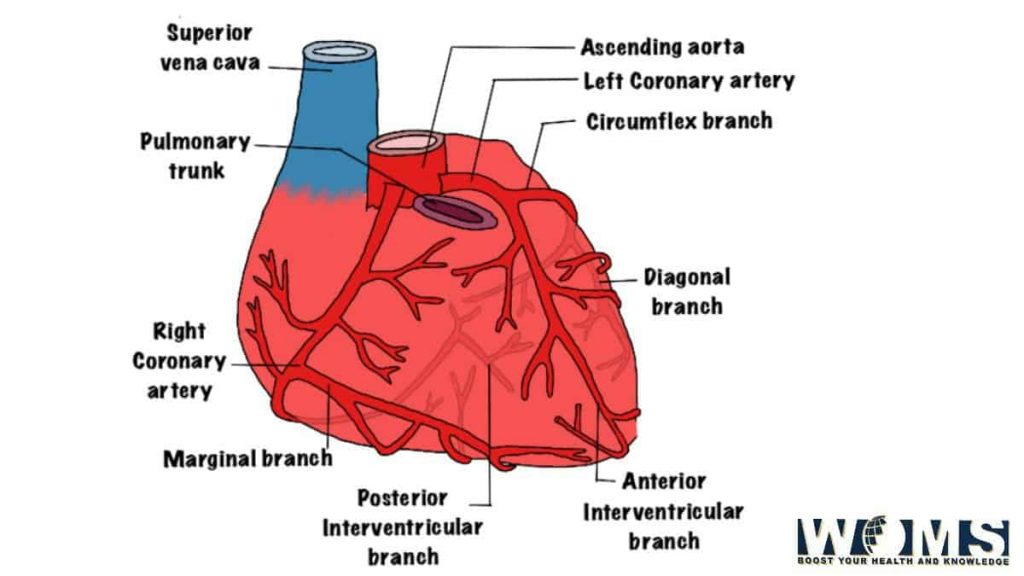
(Image Source: BD Chaursaiya)
Course
- It first passes forwards and to the right to emerge on the surface of the heart between the root of the pulmonary trunk and the right auricle.
- Then runs downwards in the right anterior coronary sulcus to the junction of the right and inferior borders of the heart.
- It winds around the inferior border to reach the diaphragmatic surface of the heart. Here it runs backward and to the left in the right posterior coronary sulcus to reach the posterior interventricular groove.
- Then it terminates by anastomosing with a circumflex branch of the left coronary artery at the crux.
Branches
- Large branches
- Marginal
- Posterior interventricular
- Small branches
- Nodal in 60% of cases.
- Right atrial
- Infundibular
- Terminal
- Right ventricular
- Conus
Conducting system
The conducting system of the heart is made up of my myocardium which is specialized for the initiation and conduction of the cardiac impulse. Its fibres are finer than other myocardial fibres and are completely cross-striated. The conducting system has the following parts.
- Sinoatrial node or SA node
- Atrioventricular node or AV node
- Atrioventricular bundle or AV bundle or bundle of HIS
- The right branch
- The left branch
- The Purkinje fibres
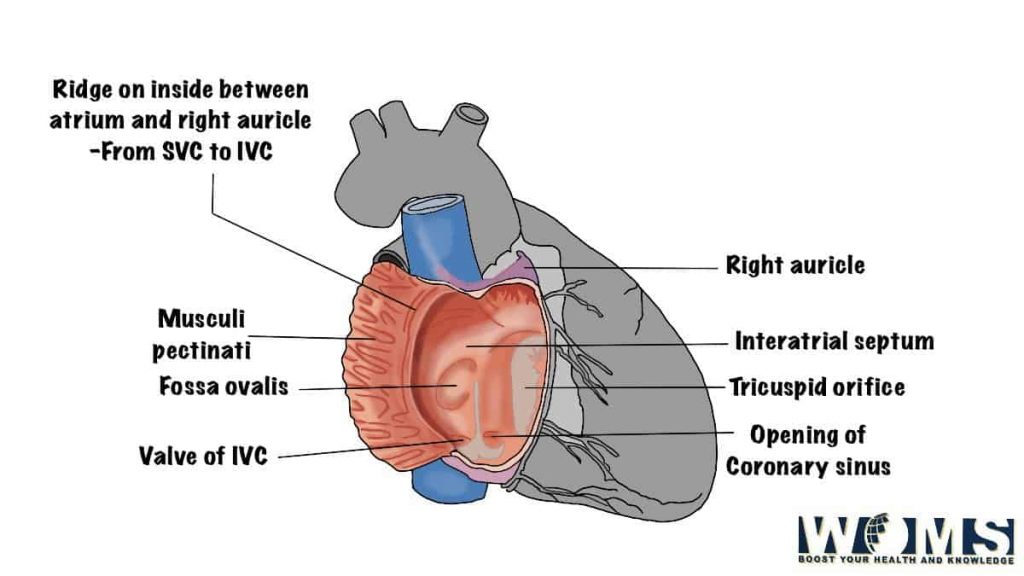
- Sinuatrial node or SA node: It is known as the ‘pacemaker of the heart. It generates impulses at the rate of about 70-100 beats/min and initiates the heartbeat. It is horseshoe-shaped and is situated at the aortocaval junction in the upper part of the sulcus terminals. The impulse travels through the atrial wall to reach the AV node.
- Atrioventricular node or AV node: It is smaller than the SA node and is situated in the lower and dorsal part of the atrial septum just above the opening of the coronary sinus. It is capable of generating impulses at a rate of about 40 to 60 beats/min.
- Atrioventricular bundle or AV bundle or bundle of His: It is the only muscular connection between the atrial and ventricular musculatures. It begins as the atrioventricular (AV) node crosses AV ring and descends along the posteroinferior border of the membranous part of the ventricular septum. At the upper border of the muscular part of the septum, it divides into right and left branches.
- The right branch of the AV bundle passes down the right side of the interventricular septum. A large part enters the moderator band to reach the anterior wall of the right ventricle where it divides into Purkinje fibres.
- The left branch of the AV bundle descends on the left side of the interventricular septum and is distributed to the left ventricle after dividing into Purkinje fibres.
- The Purkinje fibres form a subendocardial plexus They are large pale fibres striated only at their margins. They usually possess double nuclei. These generate impulses at the rate of 20-35 beats/minute.
Clinical anatomy of the heart
Cardiac arrhythmias are due to the defect of or damage to conducting systems of the heart, i.e. defects in the normal rhythm of contraction.
Except for a part of the left branch of the AV bundle supplied by the left coronary artery, the whole of the conducting system is usually supplied by the right coronary artery Vascular lesions of the heart can cause a variety of arrhythmias.
you must have pretty knowledge about the clinical anatomy of the heart. it will further help to study the surgery. you can read Bailey loves short practice of surgery.
Veins of the heart
These are the great cardiac vein, the middle cardiac vein, the right marginal vein, the posterior vein of the left ventricle, the oblique vein of the left atrium, the anterior cardiac veins, and the venae Cordis minimi. All the veins except the last two drain into the coronary sinus which opens into the right atrium. The anterior cardiac veins and the venae Cordis minimi open directly into the right atrium.
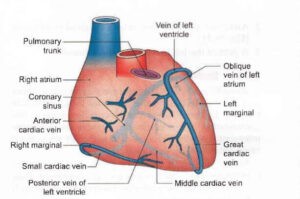
(Image Source: BD Chaursaiya)
Lymphatics of Heart
Lymphatics of the heart are associated with the coronary arteries and form two trunks. The right trunk ends in the brachiocephalic nodes and the left trunk ends in the tracheobronchial lymph nodes at the bifurcation of the trachea.
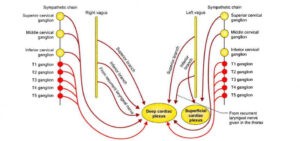
Nerve supply of heart
let’s conclude the basic anatomy of the heart with the nerve supply of the heart. Parasympathetic nerves reach the heart via the vagus. These are cardioinhibitory; on stimulation, they slow down the heart rate.
Sympathetic nerves are derived from the upper four to five thoracic segments of the spinal cord. These are cardio-acceleratory, and on stimulation, they increase the heart rate, and also dilate the coronary arteries.
Both parasympathetic and sympathetic nerves from the superficial and deep cardiac plexuses, the branches of which run along the coronary arteries to reach the myocardium.
- The superficial cardiac plexus is situated below the arch of the aorta in front of the right pulmonary artery. It is formed by :
- The superior cervical cardiac annexe of the left sympathetic chain.
The inferior cervical cardiac arm of the left vagus nerve.
The plexus is connected to the deep cardiac plexus, the right coronary artery, and to the left anterior pulmonary plexus.
The deep cardiac plexus is situated in front of the bifurcation of the trachea and behind the arch of the aorta. It is formed by all the cardiac branches derived from all the cervical and upper thoracic ganglia of the sympathetic chain, and the cardiac branches of the vagus and recurrent laryngeal nerves, except those which form the superficial plexus distribute branches to the corresponding coronary and pulmonary plexuses. Separate branches are given to the artia.
Developmental components
- Right atrium
- Rough anterior part-atrial chamber proper.
- Smooth posterior part- consumption of right horn of sinus venosus, interatrial septum
- Demarcating part-crista termanalis.
- Left atrium
- Rough part-atrial chamber proper
- Smooth part- Digestion of pulmonary veins, interatrial septum.
- Right ventricle
- The rough part-proximal portion of bulbus cordis
- Smooth part-the CONUS cordis or middle administer of bulbus cordis
- Left ventricle
- Rough part-whole primitive ventricular chamber
- The CONUS cordis or the middle portion of bulbus cordis forms the smooth part.
- Interracial septum
- Septum primum-fossa ovalis
- Septum Secundum-limbus fossa ovalis
- Interventricular septum
- Thick muscular in the lower part by two ventricles.
- Thin membranous in the upper part by fusion of inferior atrioventricular cushion and right and left CONUS swelling. Membranous part not only separates the two ventricles but also separates the right atrium from the left ventricle.
- Truncus arteriosusor distal part of bulbus cordis forms the ascending aorta and pulmonary trunk, as separated by a spiral septum.
The spiral septum is responsible for the triple reaction of ascending aorta or pulmonary trunk. In the beginning pulmonary trunk is anterior to ascending aorta, then it is to the left and finally, the right pulmonary artery is posterior to ascending aorta.
The heart is fully functional at the end of the second month of intrauterine life.
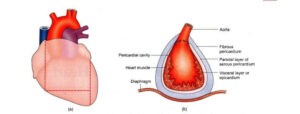
Pericardium
Pericardium, comprising fibrous and serous layers, do the heart pulsating from ‘womb to tomb Heart is a vital organ, pumping blood to the entire body. Its pulsations are governed by the brain through various nerves. Since the heartbeat is felt or seen against the chest wall, it appears to be more active than the ‘quiet brain’ controlling it.
That is why there are so many songs on the heart and few on the brain. Meditation, yoga, and exercise help in regulating the heartbeat through the brain.
Dissection
The student must have basic knowledge about the direction because it makes clear while studying the anatomy of the heart. Make a vertical cut through each side of the pericardium immediately anterior to the line of the phrenic nerve. Join the lower ends of these two incisions by a transverse cut approximately 1 cm above the diaphragm.
Turn the flap of the pericardium upwards and sideways to examine the pericardial cavity. See that the turned flap comprises a fibrous and parietal layer of the visceral pericardium.
The pericardium enclosing the heart is its visceral layer. Pass a probe from the right side behind the ascending aorta and pulmonary trunk till it appears on the left just to the right of the left atrium. This probe is in the transverse sinus of the pericardium.
Lift the apex of the heart upwards. Put a finger behind the left atrium into a cul-de-sac, bounded to the right and below by inferior vena cava and above and to left by the lower-left pulmonary vein. This is the oblique sinus of pericardium Define the borders, surfaces, grooves, apex, and base of the heart.
Features
The pericardium (Greek around the heart) is a fibro serous sac that encloses the heart and the roots of the great vessels. It is situated in the middle mediastinum. It amounts to the fibrous pericardium and the serous pericardium.
Fibrous pericardium block off the heart and fuses with the vessels which enter /leave the heart. The heart is planted within the fibrous and serous pericardial sacs. As the heart develops, it invaginates itself into the serous sac, without causing any breach in its continuity.
The last part to enter is the region of atria, from where the visceral pericardium is reflected as the parietal pericardium. Thus a parietal layer of serous pericardium gets adherent to the inner surface of the fibrous pericardium, while the visceral layer of serous pericardium gets adherent to the outer layer of the heart and forms its epicardium.
Fibrous pericardium
The fibrous pericardium is a funnel-shaped sac made up of fibrous tissue. The parietal layer of the serous pericardium is attached to its deep surface. The following features of the fibrous pericardium are noteworthy.
- The apex is blunt and lies at the level of the sternal angle. It is fused with the roots of the great vessels and with the pretracheal fascia.
- The base is broad and inseparably blended with the central tendon of the diaphragm.
- Anteriorly, it is connected to the upper and lower ends of the body of the sternum by weak superior and inferior sternopericardial ligaments.
- Posteriorly, it is related to the principal bronchi, the esophagus with the nerve plexus around it, and the descending thoracic aorta.
- On each side, it is related to the mediastinal pleura, the mediastinal surface of the lung, the phrenic nerve, and the pericardiacophrenic vessels
Serious pericardium
Serous pericardium is attenuate, double-layered serous membrane lined by mesothelium. The outer layer or parietal pericardium is fused with the fibrous pericardium. The inner band or the visceral pericardium, the epicardium is fused to the heart, except along the cardiac grooves, where it is separated from the heart by blood vessels.
The two layers are continuous with each other at the roots of the great vessels, i.e. ascending aorta, pulmonary trunk, two venae cavae, and four pul-are continuous with coronary veins.
The pericardial cavity is parietal pericardium and the visceral pericardium. It contains only a thin film of serous fluid which lubricates the apposed surfaces and allows the heart to beat smoothly.
Sinuses of Pericardium
The epicardium at the roots of the great vessels is arranged in the form of two tubes. The arterial tube encloses the ascending aorta and the pulmonary trunk at the arterial end of the heart tube, and the venous tube encloses the venae cavae and pulmonary veins at the venous end of the heart tube. The passage between the two tubes is known as the transverse sinus of the pericardium.
During development, to begin with, the veins of the heart are crowded together. As the heart increases in size and these veins separate out, a pericardial reflection surrounds all of them and forms the oblique pericardial sinus. This cul-de-sac is posterior to the left atrium.
The transverse sinus is a horizontal gap between the arterial and venous ends of the heart tube. It is bounded anteriorly by the ascending aorta and pulmonary trunk, posteriorly by the superior vena cava, and inferiorly by the left atrium; on each side, it opens into the general pericardia cavity.
The oblique sinus is a narrow gap behind the heart. It is bounded anteriorly by the left atrium, and posteriorly by the parietal pericardium and esophagus. On the right and left sides, it is bounded by reflections of pericardium as shown in fig 18.5. Below, and to the left, it opens into the rest of the pericardial cavity. The oblique sinus permits pulsations of the left atrium to take place freely
Contents of the pericardium
- Heart with cardiac vessels and nerves
- Ascending aorta
- Pulmonary trunk
- The lower half of the superior
- The terminal part of the inferior vena cava.
- The terminal parts of the pulmonary veins.
Blood Supply
You must go through the detail about the blood supply of the pericardium in the chapter on the anatomy of the heart. The fibrous and parietal pericardial are supplied by branches from:
- Internal thoracic.
- Musculophrenic arteries.
- The descending thoracic aorta.
- Veins drain into corresponding veins
Nerve Supply
The nerve supply of fibrous and parietal pericardial is phrenic nerves. They are sensitive to pain. The epicardium is supplied by autonomic nerves of the heart and is not sensitive to pain.
The pain of pericarditis originates in the parietal pericardium alone. On the other hand, cardiac pain or angina originates in the cardiac muscle or in the vessels of the heart.
Finally, the anatomy of the heart ends with these all details.
General FAQ for Anatomy of the heart
What are the four compartments of the heart?
The heart is divided into four chambers: 2 on the right side and 2 on the left side. Respectively each upper chamber is known as an atrium and each lower chamber as a ventricle. The four compartments are known as the right atrium; the right ventricle; the left atrium and the left ventricle.
Which side of the heart is the strongest?
The left and right ventricles are stronger pumps. The left ventricle is the strongest because it has to pump blood out of the entire body. When your heart functions normally, all four chambers work together in a continuous and coordinated effort to keep oxygen-rich blood circulating throughout the human body.
What are the 4 main functions of the heart?
The human heart is an organ that pumps blood throughout the body via the circulatory system,(see the conducting system of the heart in the principle article), supplying oxygen and nutrients to the tissues and removing carbon dioxide and other waste from the body.